Article • Fighting cancer together
New interdisciplinary approaches to intervention & immuno-oncology
Over recent years interventional oncology (IO), as a subspecialty of interventional radiology, has become a standard component of many cancer therapies. The broad range of minimally invasive methods – and their results – are often comparable to those of traditional approaches, such as surgery, chemotherapy or radiotherapy, e.g. with regard to hepatocellular cancer (HCC), oligometastatic diseases of the liver and the lung or small renal cell carcinoma. However, IO procedures have significantly fewer unwanted side effects as their traditional counterparts and patient acceptance is much higher.
Report: Daniela Zimmermann
Professor Thomas Helmberger, Medical Director of the Institute for Diagnostic and Interventional Radiology, Neuroradiology and Nuclear Medicine at Munich’s Klinik Bogenhausen, in Germany, outlines advances in tools for interventional oncology.
In the past decade, in addition to treatments using enzyme inhibitors, such as tyrosinkinase inhibitors, immune-modulating oncological therapies have progressed in leaps and bounds. They can support the patient’s own immune system in entirely new ways and detect and destroy tumour cells. To date, however the effects of these selective therapies remain limited and are associated with often significant side effects. ‘Interventional oncology procedures, whose immune-modulating effects so far have been considered negligible, in fact might offer substantial synergy effects when applied in combination therapies. We expect the combined application of interventional oncology and immune-oncology to overcome the limitations of the individual therapies such as merely local effects and a high degree of side effects,’ Helmberger explains. He predicts the treatment of a defined disease to continue to move towards precision medicine with the different therapy components more finely tuned to the individual patient. This hypothesis is currently being tested in several studies. ‘In these combination therapies,’ the radiologist stresses, ‘traditional surgical and minimally invasive procedures work hand in hand with individualised therapies.’
The orchestra of therapy options is increasingly complex – as is the radiologist’s task. Detailed knowledge is essential, Helmberger points out: ‘The tumour response during immuno-therapy can be quite different from the response to a conventional treatment’, thus it is crucial ‘to know these differences to be able to correctly interpret effects, such as pseudo-progression or therapy-induced pneumonitis, and take appropriate measures.’ Moreover, immuno-therapies are developing at a rapid speed – every few months new and promising immune-medication is launched that claims more specific responses or fewer side effects. ‘It’s quite a challenge to stay up-to-date,’ Helmberger admits.
From linear treatment plans to a complex therapy continuum
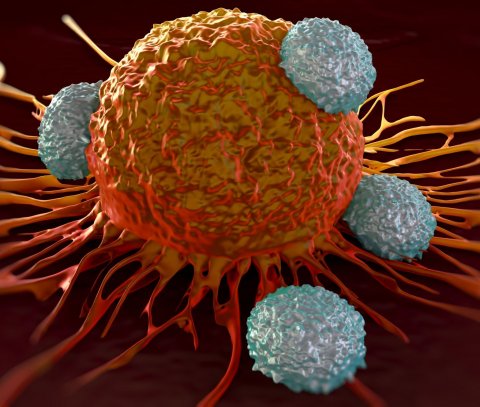
Image source: Shutterstock/royaltystockphoto.com
Increasingly complex treatment protocols are a logical consequence of better understanding of tumour biology. ‘Today we know that, on the cellular level, tumours respond differently to therapies,’ he points out. ‘Consequently, we now abandon treatment plans that assume linear courses of treatment and simple yes/no evaluations of the response in favour of more a complex therapy continuum. This means the patient is accompanied over a longer period of time and the therapy is adjusted in a more nuanced way to the actual course of the disease.’
This development has made traditional walls between disciplines more porous, he observes. ‘Oncologists, pathologists, surgeons, radiotherapists and diagnostic and interventional radiologists don’t see each other as rivals any longer, at least in larger clinics, but use interdisciplinary approaches that benefit from shared synergies.’ While this approach has not yet trickled down to every clinic, Helmberger is optimistic: ‘When the safety belt was introduced several decades ago it also took some time for everybody to be convinced of its benefits.’
AI supports human skills – if the groundwork is done properly
AI will enable us to analyse complex interdependencies and recognise links between diseases and tumour profiles that traditional statistical-analytical methods were unable to reveal
Thomas Helmberger
Helmberger expects artificial intelligence (AI) to be a game changer: ‘AI will enable us to analyse complex interdependencies and recognise links between diseases and tumour profiles that traditional statistical-analytical methods were unable to reveal.’
Today, some AI tools are being used and help, inter alia, to detect lung lesions, the extent of emphysema, or to identify the perfusion characteristics of different organs and tumours. ‘These assistants will be integrated deeper and deeper into clinical routine,’ the professor is convinced. This will yield supporting information, for example whether a suspicious spot in an MRI scan is more likely to be a tumour or a scar. In the future, patient data from different sources – radiology scans, blood analyses or histopathological information – will, Helmberger predicts, ‘be linked by intelligent algorithms that provide individualised insights into the specific course of the diseases. Processing and standardising the data required for these computational procedures will be a crucial task of medical institutions and the industry partners.’
Profile:
Radiologist Professor Thomas Helmberger MD is Medical Director of the Institute for Diagnostic and Interventional Radiology, Neuroradiology and Nuclear Medicine at Munich’s Bogenhausen hospital. His research foci are on oncological diagnostics and interventional oncology, abdominal imaging and vascular imaging and intervention. He is a member of several German and international professional associations such as the German Society for Interventional Radiology (Deutsche Gesellschaft für Interventionelle Radiologie – DeGIR), the European Society of Radiology (ESR) and Cardiovascular and Interventional Radiological Society of Europe (CIRSE). He is also an expert for several scientific publications; inter alia Hepatology, Interventional Oncology, Radiology and European Radiology.
01.07.2021