MRI will improve the treatment of wake-up strokes
Neurointensivists need to act quickly and carefully – as well as consider later complications or the psychological impact on stroke victims. This potentially debilitating disease was a central discussion among 1,400 participants from 10 countries during the three-day 29th Annual Conference of Neurointensive Medicine (ANIM), an event hosted in January by The German Society for Neuro-Intensive Care and Emergency Medicine (DGNI) and the German Stroke Society (DSG).

The ANIM 2012 Conference Secretary, Dr Gerhard Jan Jungehülsing, a consultant neurologist at the Clinic for Neurology at the Charité Berlin, is head of Clinical Studies at the Centre for Stroke Research (CSB). Susanne Werner of European Hospital asked the expert about new developments in stroke diagnosis and treatment.
Dr Gerhard Jan Jungehülsing believes the subject of strokes will become increasingly important because the number of stroke victims is increasing – with estimates predicting cases will more than double by 2040. Currently, about 250,000 people in Germany suffer a stroke every year. Thus, with an average survival rate of five years, the country could contain around a million stroke victims still suffering the effects. ‘Whilst the majority of German patients obviously receive prompt treatment and will not suffer any problems, or at least no major problems, around a third of patients will be left with permanent limitations or even disabilities, whilst a quarter of patients die within the first three months after suffering a stroke,’ Dr Jungehülsing pointed out.
Diagnosis and treatment
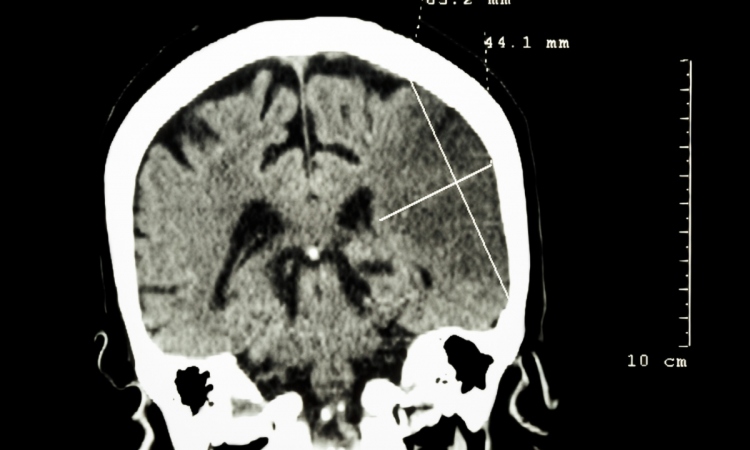
‘Stroke is a dynamic disease because the area of dying cells spreads across the brain within the first few hours of the event,’ he explained, adding therefore that the earlier its detection, the better the chances of successful treatment. ‘Complications arise when the time of the event cannot be determined. This is the case with so-called ‘wake-up strokes’ where the patient has suffered a stroke at some stage during the night and wakes up the next morning hemiplegic. In around 25% of stroke patients the exact time of the event is therefore
unclear, making treatment much more difficult. Lytic treatment for instance can only be started within 4.5 hours after the first occurrence of symptoms and therefore has not been possible for the treatment of wake-up strokes so far. Various imaging procedures will therefore play an important part in the future.’
Apart from clinical stroke studies, MRI for acute stroke is one of Dr Jungehülsing’s key scientific subjects. ‘In the future, we expect MRI will improve the treatment of wake-up strokes. We are currently investigating how to assess MRI for strokes where the time of the event is unclear. In this case, MRI is diffusion-weighted and combined with the MRI sequence FLAIR, which makes it possible to differentiate between free fluids and tissue fluids. This protocol could make the tissue damage visible, which has already occurred, and could also help to narrow down the time of event.
‘Helped by this information, we can then decide which wake-up stroke patients can receive lytic therapy and which can’t. Both CT and MRI are basically important in stroke diagnosis. Which procedure is chosen is a matter of availability. Head CT remains the method of choice to rule out brain bleeds. New perfusion CT and CT-angio procedures work even more sensitively and deliver more information. However, with the help of MRI it’s possible to determine more precisely the extent and localisation of tissue damage.’
Does MRI deliver additional information that expands the treatment spectrum?
‘We assume this is at least the case for wake-up strokes, and we will start a multi-centre study on this topic this spring. Different stroke centres nationally are working together, with our University Hospital Hamburg colleagues managing the project. We want to find out if MRI can deliver additional information on the exact time of the event for wake-up stroke patients. This data could lead to a more targeted, individualised treatment plan. My prognosis is that MRI will be used more comprehensively to treat stroke patients in the future and that the treatment spectrum will therefore expand.
CT and MRI deliver more details for the diagnosis. What part do they play when it comes to treatment?
‘Neurothrombectomy is becoming increasingly established as an alternative to lytic therapy. With this procedure, doctors remove the clot mechanically from the cerebral vessel with the help of a catheter. This is often more efficient, particularly in the case of large or proximal occlusions. Whether or not better recanalisation also means a better result for the patient is currently being investigated in a number of international studies.
The central issue is that processes in the entire field of stroke- and neurointensive medicine must be well organised. No individual medical discipline can accomplish such an intervention on its own. Everybody has to work together well - emergency medics, neurologists, anaesthetists and interventionalists. In an ideal situation, the neurologist controls the catheter and guides it into the brain. However, given a choice, it is important that this task is carried out by the person in a team with the most experience in the matter and who has carried out the most procedures.’
STEMO
At ANIM 2012, Berlin’s Stroke Emergency Mobile Unit (STEMO) was introduced to attending interventionalists. This ambulance is additionally equipped with a CT scanner. The vehicle brings the technology to the patient, saving time and helping to accurately assess the emergency, he explained. ‘Patients can then be transferred to a specialised hospital where they will receive the best possible care – more quickly. The ambulance crew is interdisciplinary. The neurologist must also be an emergency medic, and one of the emergency medical technicians must be either a trained radiographer or must have had training in radiation protection.’
23.02.2012