© Design Cells – stock.adobe.com
News • Immunology
Researchers discover new type of anticancer T-cell
A new subtype of T-cell has been discovered, which scientists hope could be used to train the immune system to tackle cancer cells in the future.
Published in the Journal of Clinical Investigation, the team from Cardiff University showed that all individuals have capacity to make anticancer T-cells that recognise cancer cells through a molecule called MR1 (MHC Class I-related Molecule 1). The new T-cell subtype, which everyone has the capacity to make, may unlock future potential to harness our own immune system to treat cancer through immunotherapy or vaccinations. These newly discovered T-cells incorporate a specific ‘signature’ that allows them to be identified across the population. The researchers believe that this subtype of T-cell is capable of sensing differences in the metabolism that occur when cells become cancerous.
Our study is important as it has identified that our results are relevant across the population as everybody can make this new T-cell subset
Andrew Sewell
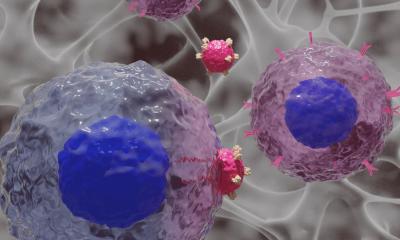
MR1 is a protein that plays an important role in allowing the immune system to identify cells infected by microbes. During an infection, the MR1 protein is presented on the surface of the infected cell where it displays a molecule called a metabolite from the infecting microbes, identifying it for destruction by T-cells.
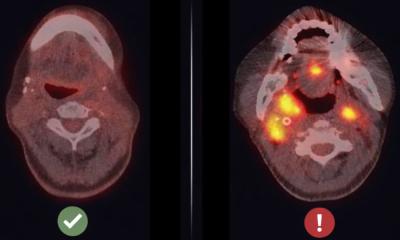
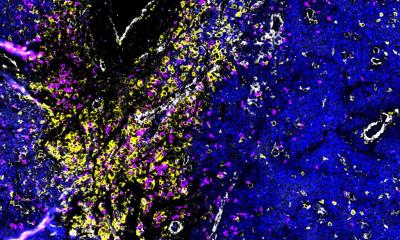
In the new study the researchers looked for T-cells that could respond to cancer cells via the MR1 protein, without attacking normal healthy cells. They sampled T-cell populations from 10 healthy donors and a patient with acute myeloid leukaemia and were able to stimulate T-cells that killed cancer cells through the MR1 molecule from the blood of all donors. These anticancer T-cells from different donors were found to have a specific signature, suggesting that they recognise the same molecule displayed by MR1 on different types of cancer cells identifying them for destruction. Importantly, this molecule must be absent or reduced on healthy cells allowing them to be ignored.
"Our study is important as it has identified that our results are relevant across the population as everybody can make this new T-cell subset. The newly identified ‘signature’ has allowed us to show what other researchers have seen - these cells inside the cancers of some patients where they express activation markers that suggest that they have attacked cancer cells," says Professor Andrew Sewell, from the University's Division of Infection and Immunity and senior author of the new study.
"Whilst our experiments suggest that our new cancer-activated T-cells recognise metabolic aspects of cancer cells in a similar way to how T-cells recognise a bacterial infection via MR1, we are not yet sure of the nature of this metabolic compound. Further experiments will be required to confirm these early observations. Identification of the compound that MR1 presents to these T-cells and that allows them to kill cancer cells while remaining inert to healthy cells will be an important next step," adds the study's co-first author Dr Hannah Thomas, also from the Division of Infection and Immunity.
The research was funded by the Wellcome Trust and the Cancer Grand Challenges partnership, Cancer Research UK, the National Cancer Institute, and the Mark Foundation for Cancer Research.
Source: Cardiff University
06.01.2025