MR diffusion and perfusion
Can they replace PET?
By Marco Essig MD, Professor of Radiology at the German Cancer Research Centre, outlines relevant presentations at the ECR.
While, in the past, MRI was praised mainly for its superb anatomic display and tissue contrast, a number of advanced, non-enhanced and contrast enhanced MR imaging techniques have been developed within the past years that provide new insights into the physiology of tissues and the pathophysiology e.g. of tumours. These techniques include MR-spectroscopy, perfusion MR imaging, dynamic contrast enhanced MRI and diffusion tensor MR.
At the ECR, in a new horizon session, on Friday morning, perfusion and diffusion MRI and their potential in oncological imaging will be described and the provocative question of whether they can replace PET will be discussed on the basis of the latest results from PET and PET-CT, presented by Professor Steinert from Zürich.
Today, the combined PET-CT acquisition is becoming the standard to assess focal and systemic cancer. PET-CT provides an excellent combination of morphological and metabolic imaging and, for example, can identify metastases that are 5 mm in diameter or larger, thanks to metabolic uptake of fluorine-18 FDG. The addition of anatomical information from CT then allows practitioners to precisely locate those metastases. However, lesions that are smaller than 5 mm cannot be detected reliably. This is one area where MRI could perhaps aim to compete. However, whilst FDG-PET is the standard tracer method in most cancer types, alternative tracers with a more specific uptake are being investigated and may enable better imaging of anti-tumour effects involving angiogenesis, apoptosis and reporter gene expression.
Should we see the modalities as rivals and how can they stimulate each other? What can functional MRI learn from PET and vice versa? Another key question for the radiological community, for the panel discussion, is how and when to use MRI instead of PET.
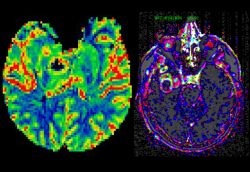
Prof. Herneth (Vienna) will present his results on diffusion weighted imaging in the assessment of lymph node metastases. DTI is a promising new methodology that allows insight into the integrity of tissue, not only of the brain. Lymph node imaging and prostate cancer are good examples to prove the potential use of this method in the description of tumour infiltration. Later in the session Dr. Berger (Munich) will explain how perfusion MRI may assess treatment monitoring in anti-cancer therapy. As at initiation, tumours in a pre-vascular phase are supplied by oxygen and nutrients that diffuse from pre-existing normal vessels, ischemia leads to the secretion of angiogenic factors when the tumour reaches a critical size. These factors, such as vascular endothelial growth factor (VEGF), recruit and maintain tumour vessels that exhibit increased blood volume and permeability compared with normal vessels. MR-based techniques, such as dynamic susceptibility weighted (DSC) MRI or dynamic contrast enhanced (DCE) MRI can be used to measure the blood volume, the vascularity, size of the vascular space within designated areas, and behaviour of contrast within those vessels. DCE-MRI has been investigated for a range of clinical oncologic applications including cancer detection, diagnosis, staging and assessment of treatment response. Tumour microvascular measurements by DCE and DSC-MRI have been found to correlate with prognostic factors such as tumour grade, microvessel density (MVD), and vascular endothelial growth factor expression (VEGF) and with recurrence and survival outcomes (Figure 1).
In addition, changes of DCE-MRI in follow-up studies during therapeutic intervention have been shown to correlate with outcome, suggesting a role for DCE-MRI as a predictive marker. The Munich researchers are trying to find out whether perfusion MRI can monitor the efficacy of anti-angiogenic treatment in kidney cancer. This type of cancer has been shown to respond particularly well to anti-angiogenic drugs. Functional measurements related to the tumour blood supply should provide a surrogate marker of whether the treatment strategy is working. This may not necessarily be obvious from measurements of the tumour size or morphology.
Work to standardise and quantify diffusion and perfusion MRI procedures is just beginning. This will be most essential if multi-centre trials are to be conducted. Dr. Stieltjes (Heidelberg), an expert in quantification strategies for structural and functional MRI techniques, will give a brief overview of how MRI data can be reliably quantified to allow them to be used for follow-up assessments and in clinical trials. Both, DTI and PWI require specifically tuned sequences and extensive post-processing. In his presentation he will illustrate the importance of both sequence development and post-processing, by going through this process for DTI (Fig. 2). The availability of different measurement techniques and their applications will be addressed. Also, he will highlight common pitfalls in DTI quantification and potential approaches to overcome
these issues.
05.03.2008





