
Source: Northwestern University
Article • Monitoring
Hybrid materials advance wearable devices
Researchers are developing wearable devices to catch early signs and symptoms of diseases or monitor sick patients. We spoke to wearables and medical device expert Professor John Rogers about the benefits, challenges, trends and innovation within the sector.
Report: Mark Nicholls
Wearable devices for monitoring patients and disease diagnosis are delivering significant advances in medicine by making continuous data available to physicians. Yet the sector faces a range of challenges as it strives to deliver cost-effective, patient-friendly products. Core to that is material selection, patient compliance, and development of smaller and less intrusive devices.
Biomedical engineering experts at Northwestern University have a growing reputation in developing smaller, more accurate, wireless, as well as battery-free devices for continuous monitoring of blood flow, blood pressure, blood oxygenation, temperature and heartbeat in patients.
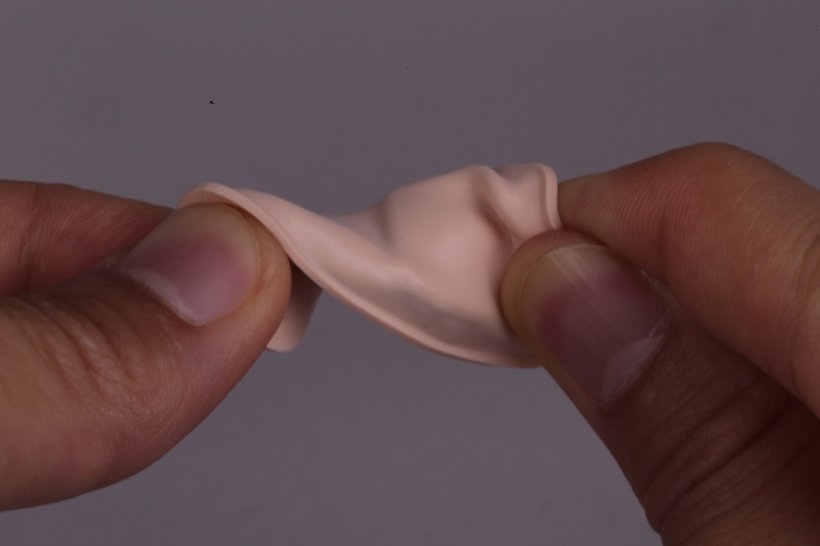
But to create cheaper, scalable devices, means a compromise of dovetailing new materials with existing technologies. This involves embracing existing rigid silicon-wafer style materials and adapting them into softer formats, paving the way for cost-effective manufacturing potential.
Patient compliancy

John Rogers, the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering and Neurological Surgery at Northwestern University, remains acutely aware that the patient interface, and compliancy, is paramount. “As engineers, we strive for design and material selections that yield devices that are physically imperceptible to the user,” he said. “If the device creates any sort of irritation or discomfort at the skin interfaces, most patients will not use it. You can develop a fantastic device with spectacular measurement capabilities, but it is meaningless if patients are unable or unwilling to use it.”
With devices needing to be softer, lighter, thinner and smaller, making them almost unnoticeable and eradicating any kind of irritation with the skin remains an enormous challenge. Current electronics are based on silicon wafers, which, while “great pieces of material technology”, are brittle and do not sit easily on the body.
“We need a fundamental change in the form factor to allow intimate, persistent physical contact with the skin,” said Professor Rogers. “The skin can serve as an excellent measurement window into a range of underlying body processes. That skin interface can generate data streams that physicians understand and can act upon. The skin is not only soft, it is very sensitive and flexible. So devices that sit on the skin must bend and move and deform with those natural motions, without constraint or slippage.”
Hybrid materials
That has seen material scientists move from silicon wafer-based electronics to explore plastic-based electronics and polymer-based conductors, whilst accounting for the practical considerations of manufacturing infrastructure.
As that is well-developed with silicon electronics, the trend has been to use the existing technology and reformulate it to yield devices that offer biocompatible mechanics. The solution: “We mix and match different types of materials,” explained Professor Rogers. “We use silicon and related compound semiconductors to support the electronics, but we structure these materials in open mesh architectures. We also embed everything in soft silicone elastomers - combining the hard rigid materials with soft flexible materials in a hybrid formation. This type of scheme can produce high performance operation in ways that exploit the sophistication and engineering options in manufacturing that already serve the consumer gadgetry industry, but morphed in a way that yields devices that are more compatible for the skin.”
That delivers the softer, flexible material that patients will be less resistant to with the cost benefits of existing manufacturing.
Source: Northwestern University
Deployable outcomes
He believes that the result offers “outcomes that are deployable today and scalable into the future”, as well as make such technologies available to lower- and middle-income countries (LMICs).
The Querrey Simpson Institute for Bioelectronics at Northwestern brings together the engineering and medical communities to develop new technologies of this sort to improve patient care and reduce costs so they are deployable effectively in both resource rich environments and have applications in LMICs. Biomedical, material science, and electrical engineers, work closely with NGOs and organisations such as the Bill and Melinda Gates Foundation and the Save the Children charity to advance this technology.
With a main campus at Evanston acting as centroid of engineering activities, plus labs in the major medical complexes of Chicago, the unit has ongoing trials of devices in areas such as cardiology, neurology, neonatology, pediatrics, nephrology, and dermatology. Patients with heart failure, cardiomyopathy, and coronary artery disease also benefit from this type of monitoring as well as stroke survivors.
“Close collaborations with physicians and nurses help us understand what the unmet needs are in current care and also provide feedback on how the devices are operating,” he added. The devices are primarily minimally invasive platforms of electronics in the style of a band-aid strip on the skin containing an array of photodetectors and light-emitting diodes, to monitor patient data.
Supporting vulnerable patients
A particular emphasis is on working with vulnerable patients at both ends of the spectrum: in neonatal pediatric health and elderly patients. Neonates, he said, are a major challenge because of the sensitivity of the skin, and small limbs and muscles. “We have developed our most sophisticated platforms for that class of patient,” he explained.
In the form of band-aid style devices applied to relevant parts of the anatomy, they are battery-free and use wireless power and data transfer, dispensing of the “primitive and constraining technology” of cables to allow critical skin-to-skin contact to continue between mother and child.
With high mortality during childbirth in LMICs these devices, piloted in Chicago hospitals, have been applied in resource-limited countries such as Zambia, Ghana and Kenya, with wireless devices measuring the cardiac health of the mother, foetus, and of the neonate immediately after birth.
With cardiac monitoring, a small device on the chest and another on the hand or foot – even in babies - can measure circulatory behaviour, differences in temperature between the core and periphery of the body, blood oxygenation and other parameters associated with haemodynamics.
A recent study in Zambia, funded by the Gates Foundation, assessed wireless monitoring of the cardiac health of 487 mothers and the foetus during birth.
Cost-effective technologies

This is where cost-effectiveness, and the value of utilising existing technologies and infrastructure, is most apparent. Smartphones can be used as monitors, and they can upload data from the rechargeable devices to the cloud. From this application for monitoring cardiac health during birth in LMCs, the Northwestern team (working with George Washington University) is also developing advanced surgical tools and implants at the other end of the cardiology spectrum.
A new class of medical instruments equipped with advanced soft electronics to apply flexible matrices of electrode sensors to balloon catheter systems used in minimally-invasive surgeries or ablations has been pioneered. Underpinning the application of internal and external devices is the need to harvest the high quality, multimodal, continuous data – the crucial information that allows physicians to diagnose and treat patients, leading to better clinical outcomes.
PROFILE:
John Rogers is the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering and Neurological Surgery, at Northwestern University in Chicago. With a focus on nano and molecular scale fabrication, characteristics of soft materials, bio-inspired and bio-integrated technologies, skin-mounted wearables and electronic implants, his research aims to better understand characteristics of ‘soft’ materials and their electronic and photonic responses for use in devices.
04.04.2022





