Article • Lung cancer screening controversy
High costs prevent programmed scans
Lung cancer is the cancer that causes the highest mortality worldwide, claiming an estimated 1.7 million patients annually, with 270,000 of those deaths in Europe.
Report: Michael Krassnitzer

According to statistics, in 2012, 3,673 people died from lung cancer in Austria alone. Why such large numbers? The first symptoms of this disease only show up once the cancer is already at an advanced stage. The five-year survival rate is just 15%.
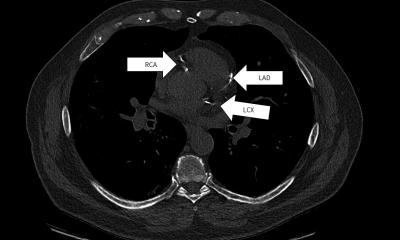
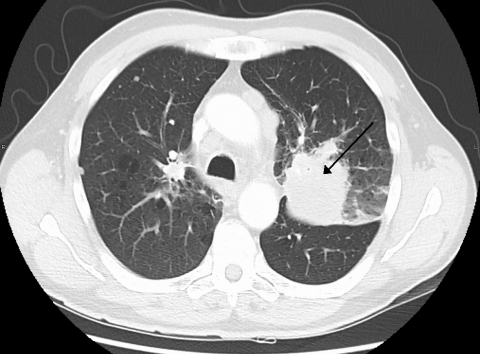
Thus the notion of a screening programme, such as regular CT scans for those at risk, appears to be obvious. The assumption is that it should help to diagnose and treat many cases of lung cancer at an earlier stage. ‘Although, at first glance, lung cancer screening may seem an obvious concept, introducing this type of programme is controversial,’ explains Professor Stefan Diederich, Senior Consultant at the Institute for Diagnostic and Interventional Radiology at the Marien Hospital Düsseldorf, and President of the International Cancer Imaging Society (ICIS). This type of screening programme and the respective recommendations are available in the USA, but not in Europe.
In the 1960s and 70s, breast cancer studies were carried out into the benefits of screening. Several randomised studies, which in those days were based on chest X-rays, showed that screening programmes significantly increased the number of cases of lung cancer being discovered at an earlier stage, but patients saw no benefits: Screening did not lower the mortality rate.
Studies carried out in the 1990s, based on CT scans, showed the same result. Although more cases of cancer were discovered at an earlier stage no effect was seen on mortality. Only in 2010, when the USA’s National Lung Screening Trial (NLST) was published, was there evidence that screening lowers mortality.
However, European studies have not yet been able to confirm the respective effect. This apparently also applies to the Dutch-Belgian NELSON Study, carried out from 2003-2012, with no results yet comprehensively published. Diederich knows the reason: The NLST study participants were at a higher risk right from the start because they were older and consumed more tobacco. At the start of the NLST study the participants were aged between 55 and 74 and had been smoking for at least 30 pack years, i.e. the number of cigarette packs consumed per day multiplied by the number of years smoked, whilst the participants in the Nelson study, as well as other European studies, were aged between 50 and 74 at the beginning and were included from 15 pack years upwards.
The consequences of the NLST study in the USA were acknowledged and lung cancer screening for those with more than 30 pack years was introduced. Not so in Europe. ’There is not a single screening programme in Europe and no efforts to introduce one either,’ Diederich points out. Ostensibly, this is because not one European study has yet been able to demonstrate the benefit of lung cancer screening. However, the truth is probably somewhat different. ‘The real issue is around the costs involved,’ the radiologist believes. ‘Each case of lung cancer, discovered in the context of screening, results in additional costs for the healthcare system.’
If suspicious lesions are discovered during screening this leads to further diagnostic steps, all of which cost money. In addition, the cost of cancer drugs has literally soared over the last few years. ‘Screening may have its benefits for the individual,’ Diederich concludes, ‘but society as a whole is faced with higher costs.’
Profile:
Professor Stefan Diederich is Senior Consultant at the Institute for Diagnostics and Interventional Radiology at the Marien Hospital Düsseldorf. A specialist in radiological diagnostics and diagnostic radiology, he studied in Münster and Heidelberg and trained in Münster and Cambridge. He is President of the International Cancer Imaging Society (ICIS); consultant for numerous scientific publications and recipient of the Eugenie and Felix Wachsmann-Prize presented by the German Radiological Society.
04.08.2017