Women and Men
Heart Disease: same symptoms, different care
Despite messages to the contrary, most women being seen by a doctor for the first time with suspected heart disease actually experience the same classic symptoms as men, notably chest pain and shortness of breath, according to a study led by the Duke Clinical Research Institute.
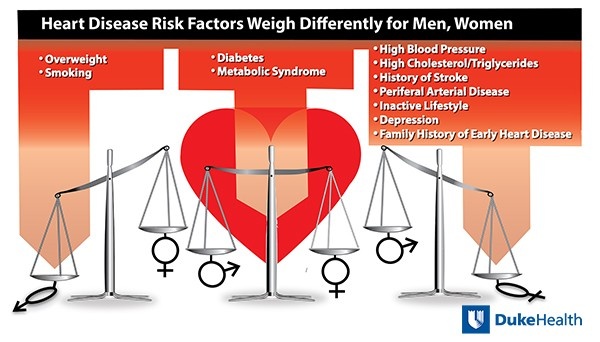
But other differences between the sexes are evident in the diagnosis and risk assessment for coronary artery disease, according to findings. “Our findings suggest there might be need for heart-health resources specifically aimed at women, because much of what is provided is for men, and there are significant sex-based differences,” said lead author Kshipra Hemal of the Duke Clinical Research Institute.
In one of the largest studies of its kind enrolling patients with suspected coronary heart diseases but without a prior history of the condition, Hemal and colleagues compared the experiences of more than 10,000 patients, evenly split between women and men, in the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (or PROMISE).
The Duke-led research team found that women have more risk factors for heart disease than men. But women are typically assessed to have lower risk. In addition, commonly used predictor models exclude issues such as depression, sedentary lifestyle and family history of early heart disease, which women report more often than men.
Women are also more likely to be referred for imaging stress tests compared to men, particularly nuclear stress testing, but they are less likely to have a positive test.
Seventy-three percent of women and 72 percent of men complained of chest pain when presenting to their physicians with suspected heart disease. Men were more likely to characterize their chest pain as a dull ache or a burning sensation, while women most often described their pain as crushing pressure or tightness.
Women were also more likely than men to have back, neck or jaw pain, and palpitations as the primary presenting symptoms, whereas men were more likely to have fatigue and weakness, although such symptoms were unusual in both sexes as the primary complaint.
Women were more likely than men to be taking beta blockers and diuretics; men were more likely than women to be taking angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers, statins, and aspirin.
“Previous studies have compared differences in demographics, risk factors, and symptom profile between men and women, but most of these focused on patients with an existing diagnosis of heart disease,” said senior author Pamela Douglas, M.D., the Ursula Geller Professor for Research in Cardiovascular Disease at Duke University School of Medicine and member of the Duke Clinical Research Institute.
“Our study is the largest of its kind looking at patients with stable chest pain or other symptoms suggestive of coronary artery disease, which is a much more common occurrence,” Douglas said. “Establishing a diagnosis is arguably more difficult among these patients. Our findings should help clarify that there are differences between men and women that we need to take into account.”
Source: Duke Health
04.04.2016