Glucose monitoring
A European perspective
Professor Oliver Schnell, of the Diabetes Research Institute, Munich, reports on discussions and findings of a panel of diabetes experts who met this summer in Switzerland
Globally, diabetes is increasing at the rate of an epidemic. In most patients, the targets for glycaemic control of diabetes, recommended in guidelines of scientific associations, are still not achieved.
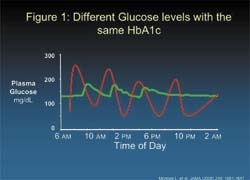
Long-term optimised diabetes management in the range of near-normoglycaemia cannot be reached without the implementation of self-monitoring of glucose monitoring (SMBG). Simply measuring HbA1c is not enough: Patients with identical HbA1c-levels may have significantly different glucose profiles (Figure 1). Both severe and smooth glucose excursions of glucose levels may result in comparable HbA1c values.
For the treatment of patients with diabetes type 2, the Global Guidelines of the International Diabetes Federation (IDF) for the European Region recommend self-monitoring of blood glucose (SMBG) in all newly-diagnosed type 2 diabetics. SMBG is also advised for people with diabetes type 2 on insulin and oral agents. The guidelines emphasise that SMBG is an integral part of self-management.
Despite the new global guidelines, Europe is still missing a homogeneous, structured and evidence-based approach across the national borders. To explore the country-specific role of glucose monitoring a Diabetes Expert Panel was held in July 2007 in Basel, Switzerland. The Panel provided an innovative forum for debate and gave insights into the practice of self-monitoring of blood glucose in different countries.
Representing Scandinavia, Professor Kari Harno, from Helsinki, said: ‘The Finish Office of Health Technology has given full support to the use of SMBG for all diabetics.’ In addition, Finland’s 2007 guidelines point out that SMBG is essential for all diabetics. ‘Compared with total healthcare costs for diabetes, the value of the test strips only amounts up to 2-4% of the entire costs,’ he added.
In Switzerland, SMBG use was threatened in 2004, when the government decided that type 2 diabetics without insulin are ineligible for reimbursement of SMBG supplies. Professor Peter Diem, of Berne, Switzerland, pointed out: ‘It took a joint effort of patients and physicians to achieve a revision of the governmental decision. Today, all type 2 diabetics in Switzerland have access to SMBG supplies.’ He attributes the success of the campaign to the fact that a joint effort was taken to provide the government with supporting evidence, including a Swiss-based cohort study. Today, including diabetics without insulin, 400 test strips per year are reimbursed.
Professor Bruno Vergès, of Dijon, France, presented data from the National ENTRED Survey 2004. In this, only 58% of type 1 diabetics tested at the recommended frequency of 3 tests/day. In type 1 diabetes, reimbursement of SMBG strips and meters is supported and 98% of people perform SMBG. Guidelines recommended SMBG ‘several times’ a day in type 2 diabetics with insulin and for educational purposes in those without insulin.
Professor Antonio Ceriello said that comprehensive national guidelines on SMBG are published by Diabetes United Kingdom. These include detailed recommendations for frequency of testing. However, local primary care trusts (PCTs) also publish their own regional guidelines for general practitioners (GPs). Generally, local PCT guidelines are restricted by budgetary constraints that limit the number of prescriptions written by GPs.
In Italy, local authorities publish their own guidelines and prevent standardisation of SMBG practices across regions. In a recent questionnaire, diabetics were asked about their SMBG practices. Up to 16% of type 1 diabetics and 21% of type 2 diabetics never check their blood
glucose levels, Prof. Antonio Ceriello reported.
Professor Peter Kempler, from Budapest said: ‘In Hungary, most type 1 diabetics are managed in specialist diabetes care centres, while type 2 diabetics are treated mostly by GPs.’ since meters and strips are prescribed mostly by specialists, the access of type 2 diabetics to glucose meters is largely limited.
Professor Oliver Schnell, of Munich, Germany added: ‘Recent legislation governing the law on healthcare for patients with public insurances has supported the reimbursement of meter testing strips for most diabetes patients.’ Currently, the diabetes community is awaiting the release of SMBG reimbursement guidelines from the German Institute for Quality and Efficiency in Health Care (IQWIG).
Another key element for Germany is that insurance companies are keen to enrol patients into Disease Management Programmes (Damps), which include strict guidelines for healthcare providers to follow.
Anne Felton, President of the Federation of European Nurses in Diabetes (FEND) and Vice-President of the International Diabetes Federation (IDF), reported that a major barrier to successful SMBG is the lack of patient knowledge in what to do with their SMBG measurements. ‘Patients need training so they know what to do if they get an abnormal blood glucose measurement,’ she pointed out; adding that fear of hypoglycaemia is another major barrier to treatment intensification by patients.
Currently, local-specific views on SMBG in diabetes appear to be a major obstacle in the implementation of well-defined use of SMBG throughout Europe. The Expert Panel made a call for future well-designed studies that assess the specific outcome of SMBG in diabetes.
Details: International Diabetes Federation. Global Guidelines for Type 2 Diabetes. 2005, www.idf.org, last access 11/9/07
30.10.2007