Global Use and Availability of Treatment Involving Transplantation of Blood Stem Cells
An examination of the world-wide use of hematopoietic stem cell transplantation (HSCT), which involves transplantation of blood stem cells derived from the bone marrow or blood, finds that there are significant differences in transplant rates between countries and continental regions by indication and donor type, and that HSCT is most frequently used in countries with higher gross national incomes and governmental health care expenditures, according to a study in the April 28 issue of JAMA.
"HSCT has become the standard of care for many patients with defined congenital or acquired disorders of the hematopoietic system [pertaining to the formation of blood cells] or with chemosensitive, radiosensitive, or immunosensitive malignancies. Over the last 2 decades, HSCT has seen rapid expansion in use and a constant evolution in its technology," the authors write. "It requires significant infrastructure and a network of specialists from all fields of medicine. Hence, information on indications, use of specific technologies, and trends in the application of HSCT is essential for correct patient counseling and for health care agencies to prepare the necessary infrastructure and to avoid planning errors." Little is known about HSCT use and the factors associated with it on a global level.
Alois Gratwohl, M.D., of University Hospital Basel, Switzerland, and colleagues conducted a study to assess differences in the application of HSCT on a global level and to examine associations of various factors with transplant rates. The study included patients receiving allogeneic (genetically different) and autologous (derived from the same individual) HSCTs for 2006, collected by 1,327 centers in 71 participating countries of the Worldwide Network for Blood and Marrow Transplantation. The regional areas used in this study were (1) the Americas (the corresponding World Health Organization regions are North and South America); (2) Asia (Southeast Asia and the Western Pacific Region, which includes Australia and New Zealand); (3) Europe (includes Turkey and Israel); and (4) the Eastern Mediterranean and Africa.
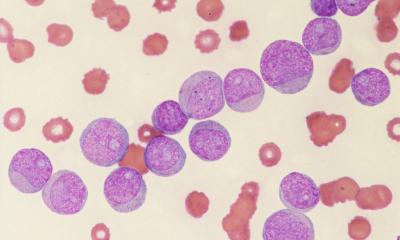
A total of 50,417 first HSCTs were reported for 2006; 43 percent were allogeneic, 57 percent autologous. Most of the autologous HSCTs occurred in the Americas and Europe. The most frequent malignant disease for an allogeneic HSCT was acute myeloid leukemia (33 percent); the most frequent nonmalignant disease was bone marrow failure syndrome (6 percent); and the most frequent indication for an autologous HSCT was a plasma cell disorder (41 percent).
"Use of allogeneic or autologous HSCT, unrelated or family donors for allogeneic HSCT, and proportions of disease indications varied significantly between countries and regions. In linear regression analyses, government health care expenditures, HSCT team density (indicates the number of transplant teams per one million inhabitants), human development index, and gross national income per capita showed the highest associations with HSCT rates," the authors write.
Most of the 50,417 HSCTs were performed in Europe (48 percent), followed by the Americas (36 percent), Asia (14 percent), and the Eastern Mediterranean and Africa (2 percent). The median (midpoint) HSCT rates (per 10 million inhabitants) varied between the continental regions and between participating countries, from 48.5 in the Americas, 184 in Asia, 268.9 in Europe, and 47.7 in the Eastern Mediterranean and Africa. No HSCTs were performed in countries with less than 300,000 inhabitants, smaller than 960 km2, or having less than U.S. $680 gross national income per capita.
"In conclusion, this global overview on HSCT activity demonstrates that it is an accepted therapy worldwide, with different needs and priorities in different regions. Transplant activity is concentrated in countries with higher health care expenditures, higher gross national income per capita, and higher team density; hence, the availability of resources, governmental support, and access to a transplant center determine regional HSCT activity," the researchers write.
(JAMA 2010;303[16]:1617-1624)
28.04.2010