Image source: Salim M, Liu Y, Sorkhei M et al., Nature Medicine 2024 (CC BY 4.0)
Article • Risk stratification initiatives in Europe and UK
The future of breast imaging: a date with density
About 60% women in Europe enrolled in a national breast cancer screening programme who have a screening mammogram can feel reasonably confident that radiologists will be able to diagnose early-stage breast cancer. But what about the 30% categorised as having dense breasts, and the 10% who have extremely dense breasts? At the 2025 SBI (Society of Breast Imaging) Breast Imaging Symposium held in Colorado Springs, USA, Prof. Ruud Pijnappel, MD, PhD, discussed current clinical trials addressing breast screening of dense-breasted women.
Special report: Cynthia E. Keen
For these women, detecting early-stage breast cancer on mammographic images can be challenging. They may need additional types of breast imaging,1 but which technologies are most effective? Clinical trials in Europe are underway to determine the most beneficial and most cost-effective screening methods for high-risk women. They are needed to convince governments to fund supplemental breast imaging to screen for cancer in women at average risk with dense breast tissue.
Ruud Pijnappel, Professor of Breast Radiology at the University Medical Centre (UMC) Utrecht, the Netherlands, and chief executive officer of the Dutch Expert Centre for Screening in Nijmegen, started off with a transatlantic overview: 'Research in Europe on this subject differs slightly from that being undertaken in the United States,' he said. 'One imaging methodology does not fit all, and protocols for more personalised screening are needed. Research in Europe is especially focussed on risk profiling so that interval cancer rates can be reduced, and to make screening frequency and modality based on an individual woman’s risk assessment.’
Recommended article
News • Radiomic parenchymal phenotypes
Dense breasts = high cancer risk? It's not that simple
Using radiomics on mammograms of over 30,000 women, researchers have identified six breast texture patterns that may be associated with increased cancer risk.
Between impressive evidence and financial challenges
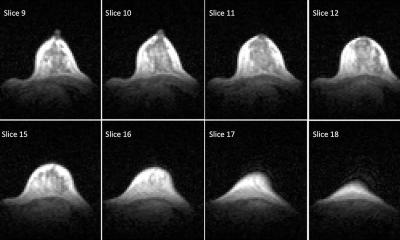
The DENSE clinical trial (NCT01315015) involves over 40,000 women ages 50 to 75 with extremely dense breasts living in the Netherlands who had normal results on screening mammography. It is evaluating if supplemental breast MRI can minimize the number of interval cancers in a two-year screening round. Participants were randomly assigned in a 1:4 ratio. For the MRI group, the interval-cancer rate was 0.83 per 1000 screenings compared to 5.06 per 1000 in the mammography-only group in the first round.2
'This solid scientific evidence was impressive, but costs and breast MRI scanner availability made this very difficult for EU countries to implement,’ explained Prof. Pijnappel. ‘Only Estonia adopted supplemental MRI screening for extremely dense breasted women to its national screening programme protocol. So, three clinical trials investigating individual screening optimisation were initiated.’
Ongoing clinical trials
Launched in November 2024, the DENSE 2 (NCT06636370) trial is enrolling 36,000 women aged 49-72 with density D category to determine if either contrast-enhanced mammography (CEM) or an abbreviated breast MRI (AB-MRI) exam supplementing a “normal results” at mammography performed at UMC Utrecht are more effective in reducing interval cancers than mammography alone. CEM is less costly and easier to implement than a conventional breast MRI. Secondary outcomes of the study include cancer detection rates and false positive rates. This trial includes two screening rounds and is expected to conclude in April 2029.
Breast cancer screening should become more personalised, not the “one size fits all” frequency of today
Ruud Pijnappel
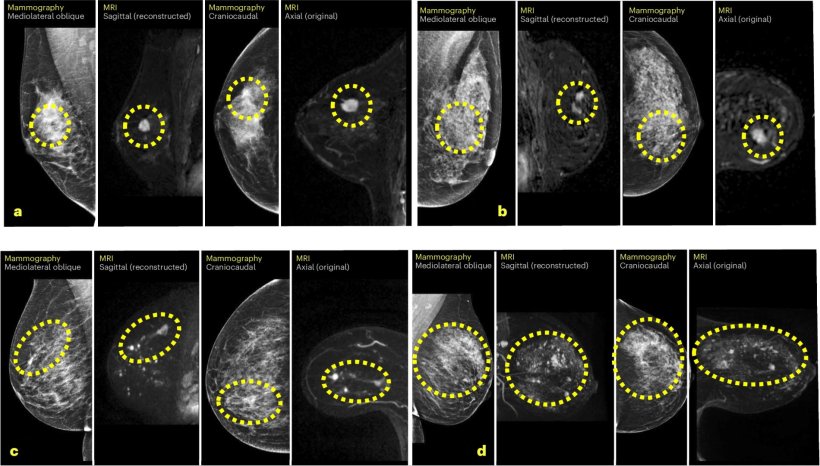
In the United Kingdom, mammography breast cancer screening is offered to women ages 50 to 75 every three years. The Breast Screening-Risk Adaptive Imaging for Density (BRAID) randomised clinical trial (NCT04097366), led by Prof. Fiona J. Gilbert, MD, of the University of Cambridge, recruited 9,361 women with C and D dense breast categories who have had a normal screening mammogram at one of 10 locations. Participants were randomised to a control group without supplemental testing, or to receive a CEM, an AB-MRI scan, or automated whole breast ultrasound (ABUS). The first supplemental exams were performed within six months of the screening mammography.3 Begun in 2019, the primary endpoint of the study is to measure both the primary and interval cancer detection rate over 42 months, recall and biopsy rates, tumour size, and grade of cancer.
Prof. Pijnappel explained that the interim results presented at ECR 2025 revealed that 85 cancers were diagnosed with supplemental screening: 73 invasive cancers and 12 ductal carcinomas in situ (DCIS). The cancer detection rate was 19.2 per 1000 examinations for CEM, 17.4% for AB-MRI, and 4.2% for ABUS. The invasive tumour size identified by AB-MRI and CEM was half the size of those found with ABUS.4
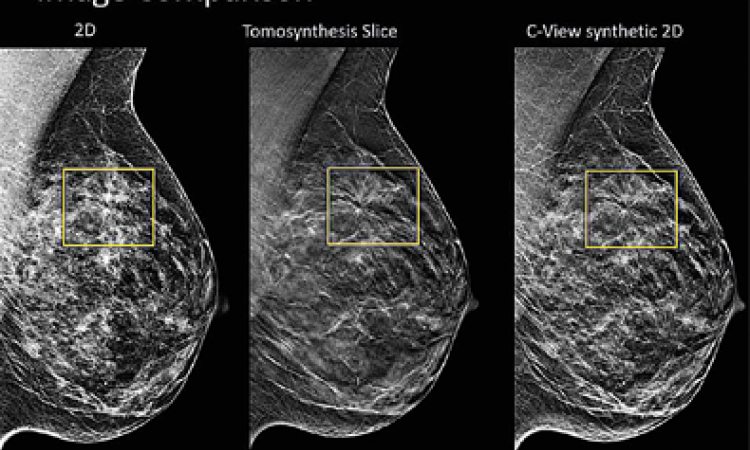
The ScreenTrustMRI (NCT04832594) prospective clinical trial being conducted at Karolinska University Hospital in Stockholm, Sweden, is evaluating the ability of an AI tool (AISmartDensity) to identify women with the highest probability of having a delay in cancer detection from a false negative screening mammogram, and who would benefit from a supplemental breast MRI exam. The AI tool assesses mammographic breast density, potential masking, suspicious cancer signs, and other risk factors.
The AI tool analysed data of 1,211 women to whom it had assigned high risk scores to mammography exams performed at Karolinska. Principal investigator Fredrik Strand, MD, PhD, advised that the cancer detection rate of participants who had a supplemental MRI was 64.4 cancerous lesions per 1,000 exams, according to a report of interim data published in Nature Medicine.
Because the AI tool only selected 6.9% of over 59,300 women, Dr Strand and colleagues state that the cost per cancer detected with supplemental MRI is four times more efficient than conventional mammography. Additionally, it is comparable to the cost of screening mammography for this very high-risk population. In a future study, the researchers will investigate if an additional review of mammograms flagged as high risk by the AI tool will yield an increased cancer detection rate.5
Appeal for a more personalised approach
Prof. Pijnappel predicts that breast cancer risk stratification by traditional density measurement is going to become less important, and that AI tools have great potential to identify at-risk women. 'Not every woman with dense breast tissue will develop cancer. And you know that breast cancer occurs in women with average tissue density and fatty breasts. Women at low risk may only need mammograms at four- or five-year intervals. This may offset the cost of offering exams annually to high-risk women. Breast cancer screening should become more personalised, not the “one size fits all” frequency of today,' he concluded.
References:
- Berg WA, Harvey JA: Breast Density and Supplemental Screening; Society of Breast Imaging; https://www.sbi-online.org/white-papers/breast-density-and-supplemental-screening. Accessed 28 July 2025.
- Bakker MF, de Lange SV, Pijnappel RM, et al.: Supplemental MRI Screening for Women with Dense Breast Tissue; N Engl J Med. 2019;381(22):2091-2102; https://doi.org/10.1056/nejmoa1903986
- Allajbeu I: Breast Screening – Risk Adapted Imaging for Density trial. CTiR11 – Clinical Trials in Radiology 1; ECR 2025, Vienna, Austria. https://connect.myesr.org/course/clinical-trials-in-radiology-1-6.
- Gilbert FJ, Payne NR, Allajbeu I, et al.: Comparison of supplemental breast cancer imaging techniques – interim results from the BRAID randomized controlled trial; Lancet 2025;405(10493):1935-1944; https://doi.org/10.1016/S0140-6736(25)00582-3
- Salim M, Liu Y, Sorkhei M, et al.: AI-based Collection of individuals for supplemental MRI in population-based breast cancer screening: the randomized screen trust MRI trial; Nature Medicine 2024;30:2623-2630; https://doi.org/10.1038/s41591-024-03093-5
Profile:
Prof. Ruud Pijnappel, MD, is Professor of Breast Radiology at UMC Utrecht and chief executive officer of the Dutch Expert Centre for Screening in Nijmegen, the Netherlands. He was President of the Dutch College of Breast Imaging from 2011 to 2015. Prof. Dr Pijnappel is secretary general and board member of several national and international workgroups engaged in research into the diagnosis and treatment of breast cancer. In addition to the Radiological Society of the Netherlands, he is a member of the European Society of Radiology (ESR), the Society of Breast Imaging (SBI) and the European Society of Breast Imaging (EUSOBI).
03.11.2025