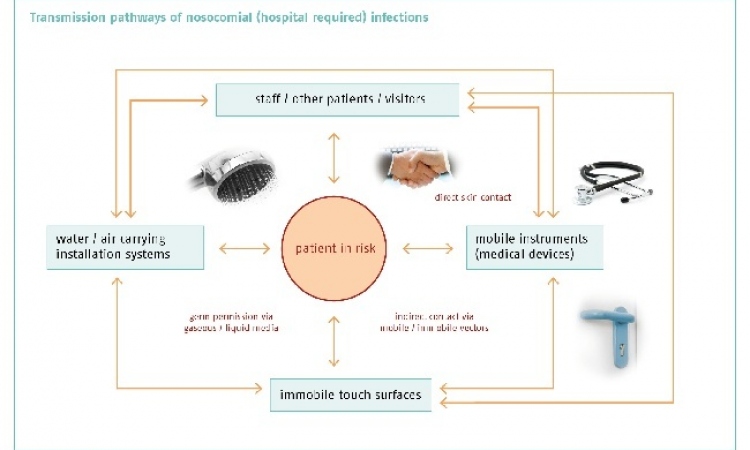
Focus: hygiene and nosocomial infections
They are one of the major threats in today's hospital: tiny pathogens that hide out in catheters, in ventilation tubes, on instruments or on the keyboards of medical technological equipment only waiting to attack patients whose immune system is already weakened. This week, EH Online will take a closer look at nosocomial infections, their causes, their effects and the available ways and means to fight them.
An airflow system might protect against infections.
The numbers are frightening: according to the European Centre for Disease Prevention and Control in European hospitals each year three million patients acquire an infection. In Italy, between 4.500 and 7.000 patients who turned to their hospital for medical help, die of nosocomial infections each year while in Germany the figure is estimated to be between 10,000 an 15,000. And in the US the annual death toll is 44,000 to 98,000.
Even worse is the forecast: The number of deadly pathogens will increase over the next few years – despite medical progress – because on average, patients will be older, their immune systems already weakened while at the same time the number of therapies these patients undergo will increase and thus their immune system will be even further compromised. Moreover, with complex medical instruments entering the human body ever deeper the infection risk is also rising. And last not least during the last two decades we have witnessed the – often enough uncalled for – use of antibiotics skyrocket, a fact which contributed to the development of resistance.
see also:
Advertisement
Indeed, nosocomial infections account for a large percentage of the clinical complications occurring during hospital stays. When a patient acquires an infection and stays in the hospital weeks or even months longer than anticipated, hospitals which are reimbursed based on diagnosis related groups are seldom paid for the additional stay and care. The average costs of patients who develop an infection are nearly four times higher than for patients admitted with the same diagnosis and severity of illness who did not contract an infection. And: in the future, the occurrence rate of nosocomial infections will be an important quality indicator for clinical and nursing care.
In Germany, the data collected by the Krankenhaus-Infektions-Surveillance-System (KISS) show that approx. 30,000 patients in ICUs acquire pneumonia. In most cases the bacteria enter the patient’s body via the mouth – indicating a lack of hygiene. Gloves that were not changed after use, improperly cleaned ventilation tubes, an improperly disinfected instrument – these seemingly benign mistakes allow the pathogens to colonize a human body. Physicians and nursing staff transmit the bacteria.
Today, there is hardly a hospital which has not introduced stringent measures to fight the bacteria: the use of antimicrobial equipment is exploding. According to market researcher Frost&Sullivan, in 2007 the European market for sterilisation and disinfectant equipment grew to 269.7 million USD. For 2014 an increase to 352.0 million USD is expected – an annual growth rate of 3.9 percent.
Antimicrobial displays by Totoku, key boards like those offered by Devlin or an airflow system by Normeditec - all these innovations that EH Online presents this week were designed to reduce the infection risk. “Within a few minutes meticulously sterilised instruments and implants can be contaminated by micro-organisms“, says Normeditec. The company’s airflow system Toul however, which is placed right next to the operating table, can reduce bacterial load on the operating field and the instrument table by 95 percent.
But innovative products won’t suffice to manage the problem. Training for physicians and nursing staff regarding prevention strategies are hospital management tools which are as crucial as the scientific research on new antibiotics.
The most dreaded among the dangerous bacteria is MRSA - methicillin-resistant Staphylococcus aureus. Today, MRSA is basically resistant against all commercially available antibiotics. Even vancomycin, the usual „emergency“ antibiotic, can not always kill this tenacious micro-organism. Traditional antibiotics destroy the microbe by crushing its cell wall. Except MRSA. Last July a research team of the University of Notre Dame in the US discovered that MRSA carries on its surface a unique protein called penicillin-binding protein 2a (PBP 2a) which makes sure that the antibiotic cannot destroy its cell wall. That explains why MRSA is antibiotic-resistant. In their study, the scientists showed that an innovative antibiotic developed by the bio-pharmaceutical company Cerexa interacts in a unique way with PBP 2a. Finally, this knowledge might pave the way for the development of an effective weapon against MRSA.
12.08.2008
More on the subject: