Fatty acids may shield young from type 1 diabetes
Omega-3 may protect children at high risk of developing type 1 diabetes, according to a study published in the Journal of the American Medical Association.
The incidence of type 1 diabetes among 1,770 children at high risk of developing this disease, with increased omega-3 intake associated with a 55 per cent reduction in risk, was investigated by researchers at the University of Colorado, in Denver, the University of Florida and Roche Molecular Systems. ‘Our study suggests that higher consumption of total omega-3 fatty acids, which was reported on the FFQ, is associated with a lower risk of islet autoimmunity (IA) in children at increased genetic risk of type 1 diabetes,’ said lead author Jill Norris, at the University of Colorado. ‘This association is further substantiated by the observation that a higher proportion of omega-3 fatty acids in the erythrocyte membranes is associated with a decreased risk of IA in a subset of this same population.’
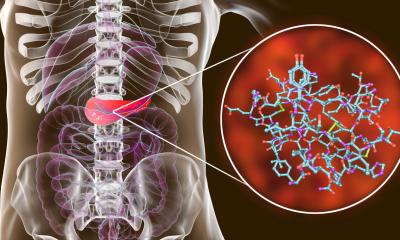
The authors explained that type 1 diabetes mellitus is an autoimmune disease characterised by the destruction of insulin-producing beta cells in the pancreatic islets. ‘Although it is not yet known what initiates the autoimmune process, it is likely that both genetic background and environmental factors contribute to the disease process.’ To investigate the potential dietary contribution in the development of type-1 diabetes, the researchers examined whether consumption of omega-3 and omega-6 fatty acids was associated with the development of pancreatic islet autoimmunity (IA). Dietary intakes were evaluated using a 111-item food frequency questionnaire (FFQ) completed annually by the children’s mothers. Two-year-old children were recruited and followed for a 6.2-years average. Children were identified as having a high risk of type 1 diabetes by either possessing a high diabetes risk HLA (human leukocyte antigen) genotype or having a sibling or parent with type 1 diabetes.
To investigate the risk of IA related to the levels of polyunsaturated fatty acids in red blood cell (erythrocyte) membranes, a case-cohort study was also carried out with a subset of 244 children. During the follow up period, in the total study population the researchers documented 58 positive cases of IA and, after adjusting for confounding factors that included HLA genotype, family history of type 1 diabetes, caloric intake, and total omega-6 fatty acid intake, found that total omega-3 fatty acid intake was inversely associated with a 55% reduction in IA risk.
In the case-cohort study, omega-3 fatty acid content of erythrocyte membranes was associated with a 37%t decreased risk of IA. Levels of the three marine omega-3 fatty acids eicosapentaenoic acid (EPA, 20:5n-3), docosahexaenoic acid (DHA, 22:6n-3), and docosapentaenoic acid (DPA, 22:5n-3) were combined with the plant omega-3 alpha-linolenic acid (ALA) to estimate the total omega-3 fatty acid intake.
No direct mechanistic study was performed by the researchers, but they suggest that the benefits of the omega-3 fatty acids may be due to their anti-inflammatory properties, and their ability to reduce oxidative stress. ‘Overall, our data suggest that ingestion of omega-3 fatty acids throughout childhood may decrease the risk of IA,’ they concluded.
If a new clinical trial - The Nutritional Intervention for the Prevention of Type 1 Diabetes – confirms that anti-inflammatory doses of DHA during pregnancy and infancy could inhibit early islet inflammatory events key to the development of type-1 diabetes, the researchers think omega-3 fatty acids supplements could become a mainstay for early intervention to prevent type 1 diabetes from developing.
Source: Journal of the American Medical Association (26/907. Vol. 298, N. 12). Omega-3 Polyunsaturated Fatty Acid Intake and Islet Autoimmunity in Children at Increased Risk for Type 1 Diabetes. Authors: Jill M Norris, X Yin, M M Lamb, K Barriga, J Seifert,
M. Hoffman, H D Orton, A E Baron,
M Clare-Salzler, H P Chase, N J Szabo,
H Erlich, G S Eisenbarth, M Rewers
30.10.2007