Fatal blood clots claim 500,000 EU lives annually
by Ian Mason
Experts call for screening of surgical and medical patients, and thromboprophylaxis for those at risk.
As hospital administrators and clinicians across Europe are urged to take action to cut these unnecessary deaths - experts call for screening of surgical and medical patients, and thromboprophylaxis for those at risk.
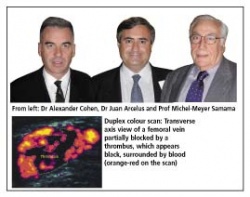
Pulmonary embolism following venous thrombosis claims over 500,000 lives in the EU annually, according to a new study. The need for preventive measures is clear, since most premature deaths due to blood clots are avoidable, says Dr Alexander Cohen, on behalf of the Venous Thrombo-embolism (VTE) Impact Assessment Group in Europe (VITAE).
‘VTE kills more Europeans each year than breast cancer, prostate cancer, HIV/AIDS and road traffic accidents combined,’ said Dr Cohen, of Guy’s, King and St Thomas School of Medicine and King’s College Hospital, London, UK. ‘The direct cost of VTE to EU healthcare systems exceeds three billion euros annually.’
Failure to prevent thrombosis is now the single most common cause of medical negligence litigation in the USA, and cases in the EU are now soaring, he cautioned.
‘Hospital administrators and clinical directors need to check they have adequate protocols in place. In many EU countries government regulators are looking closely at the problem of VTE, and audits may soon be mandatory, ‘ he added.
The VITAE study - the first major attempt to establish the burden of VTE across the whole EU - shows that the annual toll of fatal and non-fatal symptomatic VTE, which includes pulmonary embolism (PE) and deep vein thrombosis (DVT), exceeds 1.5 million events annually in the European Union. This figure includes 543,500 deaths, 435,000 cases of PE and 684,000 cases of documented symptomatic DVT.
The VTE burden is probably much higher than these figures suggest, because in many cases it is clinically silent and difficult to diagnose. Most fatal PEs remain unrecognised as post mortems are rarely performed. ‘More than 70% of fatal PEs are only detected during post-mortem examination,’ said Professor Juan Arcelus, Department of Surgery, University of Granada Medical School, Spain. Patients should be screened, and if at risk, considered for thromboprophylaxis - this includes surgical patients and medical patients with restricted mobility, such as those with myocardial infarction, heart failure, stroke, acute infection or acute rheumatological disease - it is not often appreciated but PE kills three times more medical, than surgical patients.’
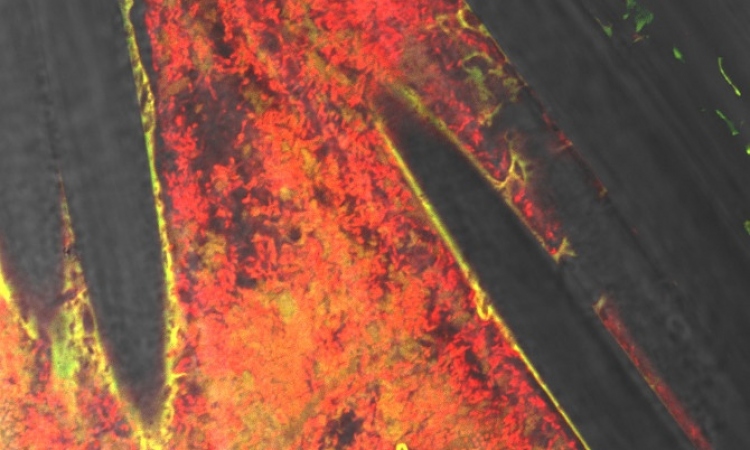
Dr Marie-Antionette Sevestre, Service de Medicine Vasculaire, CHU Amiens, France would like to see greater use made of Duplex Ultrasound Scanning in the diagnosis of DVT. ‘It is an accurate, non-invasive and cost effective technique that accurately identifies the site of the thrombus and helps stratify risk, but at the moment, many more patients who need scanning are not scanned,’ she said.
Professor Michel-Meyer Samama, Hotel-Dieu University Hospital, Paris, France, has authored several influential textbooks on clinical thrombosis and hypercoagulable states. He says that too many relatively young patients die due to lack of adequate prophylaxis. ‘VTE is a silent disease that prematurely takes live although available and effective prophylaxis and treatment exists.’
Preventive treatments for DVT include early mobilisation, sequential compression devices and stockings to prevent blood clotting, and anticoagulants and/or blood-thinning drugs.
DVT results when a blood clot inside a deep vein, commonly located in the calf and or thigh. PE a potentially life-threatening complication occurs when a fragment of a blood clot breaks loose and travels to the lungs.
Venous thrombo-embolism: The facts
Venous thromboembolism (VTE) is caused by the formation of blood clots that partially or completely block a vein. The most common form is deep vein thrombosis (DVT), occuring when clots form in deep veins, usually in the legs.
Parts of the clot may break off and lodge in the arteries that supply the lungs, forming a pulmonary embolus (PE) - a medical emergency that can cause irreversible damage to the lungs and which frequently results in death.
Risk factors for DVT and PE include: increasing age, prolonged immobility, stroke, or paralysis; previous VTE; cancer and its treatment; major surgery; trauma; obesity; varicose veins; cardiac dysfunction; and pregnancy.
The risk of developing DVT after hip replacement has been estimated to be as high as 50% of patients when thromboprophylaxis is not used. The use of thromboprophylaxis can reduce this risk to between 10 and 15% of patients.
Despite the high risk of VTE in patients undergoing major surgery, some 40% or more of these patients still do not receive effective thromboprophylaxis.
Patients who suffer DVT are at risk of developing post-thrombotic syndrome (PTS), a painful, unpleasant and potentially disabling condition often resulting in the development of leg ulcers, which are persistent and difficult to heal.
The United Kingdom’s House of Commons Health Select Committee recently published recommendations for the prevention of VTE in hospitalised patients. These included:
> On admission to hospital all patients should be counselled on the risks of VTE and undergo a risk assessment to determine if drugs should be administered
> Awareness should be raised among medical practitioners of the extent of the problem: all physicians and surgeons are to be informed if their patients contract VTE after they have been discharged from hospital
> Thrombosis committees and thrombosis teams should be established in each hospital to promote best practice and to be a source of education and training for all staff
VTE prevention
Thromboprophylaxis is available in both mechanical and pharmacological forms. For patients with moderate to low risk of blood clots mechanical prophylaxis may be used instead of, or in combination with, pharmacological prophylaxis. Mechanical methods of thromboprophylaxis include pneumatic calf compression and compression stockings.
Surgical patients (especially those undergoing orthopaedic surgery) and medical patients classified as medium or high risk may be given anticoagulants to decrease the risk of blood clots.
Pharmacological agents for thromboprophylaxis include unfractionated heparin, LMWH, thrombin inhibitors, oral anticoagulants, and specific factor Xa inhibitors.
Many surgeons now advocate that prophylaxis after joint replacement should continue after the patient is discharged from hospital (extended prophylaxis). The duration of extended prophylaxis depends on the risk category of the patient and the treatment that is undertaken.
Extended prophylaxis normally lasts for five weeks but in high-risk patients, or in those who have previously experienced DVT, prophylaxis can be administered for a significantly longer period.
In a double-blind, placebo-controlled trial the risk of DVT/PE was reduced by 63% in acutely ill medical patients treated with enoxaparin when compared with placebo, without increased major bleeding. Enoxaparin reduced the risk of VTE by up to 50% in patients undergoing high-risk surgical procedures versus unfractionated heparin.
02.08.2006