Image source: Adobe Stock/romaset
Article • Plenary discussion at ECR 2023
Sustainable radiology: why it takes more than “greener” imaging systems
Despite the strong Irish presence at this year’s ECR – courtesy of Congress President Prof Adrian Brady – it’s clear that radiology is lacking in the “green” department: healthcare still causes a large share of global greenhouse gas (GHG) emissions, not least due to diagnostic imaging. But while it might be easy to pin the blame on power-hungry CT and MRI systems, things might not be quite as clear-cut after all: Dr Sarah Sheard, Consultant radiologist at Imperial College Healthcare, UK, invited her ECR audience to take a closer look at radiology’s climate footprint – and revealed ways to make the field more sustainable.
Article: Wolfgang Behrends

© Imperial College Healthcare NHS Trust
While carbon dioxide (CO2) has become somewhat of a synonym for gases that accelerate global warming, other compounds used in healthcare have a far greater impact – such as the anaesthetic gas desflurane (C3H2F6O), or sulphur hexafluoride (SF6), which is used as a contrast agent in ultrasound imaging and has a global warming potential (GWP) 22,900 times greater than CO2. Reducing the use of these high-impact compounds can greatly contribute to “greener” practices, Dr Sheard pointed out. ‘For this reason, the NHS has announced that it will completely phase out the use of desflurane by the beginning of next year and replace it with lower-GWP anaesthetic gases.’
The huge impact of HVAC
Radiology may be largely built around the use of huge, power-hungry scanners, but the actual share of these systems on the energy consumption of a typical radiology ward is comparably small, the expert continued. ‘It is important to remember that there are other forms of environmental damage we can do through our activities.’ Recent investigation have shown that the journey of a patient through a interventional radiology unit generates substantial GHG volumes, a majority of which come not from the imaging itself, but from energy used to maintain climate control, followed by emissions related to single-use surgical supplies.1 According to this paper, HVAC – heating, ventilation and air conditioning – contributes to almost half of the total emissions (49.2%), while the energy expenditure (plug load) for imaging only makes up 2.78%. ‘A huge challenge is seeing the impact from heating and cooling our departments, especially in old, inefficient buildings,’ Dr Sheard said, pointing out the need for more energy-efficient construction and renovation.
Not all imaging is (carbon) equal
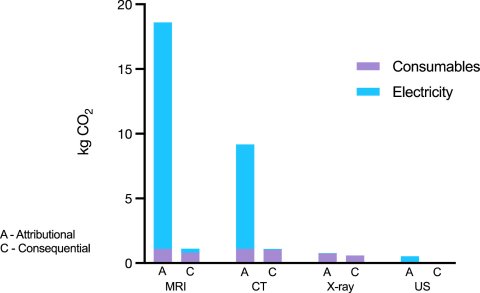
Image source: McAlister et al., Lancet Regional Health – Western Pacific 2022 (CC BY-NC-ND 4.0)
Going into more detail regarding the imaging systems, the radiologist showed that the devil is often in the details. For one, a recent study found significant variations in the carbon footprint of the most common modalities2: the average carbon emissions per scan were highest for MRI (17.5 kg CO2 equivalents), followed by CT (9.2 CO2e). By contrast, chest x-ray and ultrasound imaging generated much smaller footprints per scan, using only 0.76 and 0.53 CO2e, respectively.
Strikingly, the amount of energy used for a single scan on a previously inactive system was far greater than that for any additional scans performed on a system that was already running. This, the radiologist said, makes a strong case for operating imaging systems at full capacity whenever possible.
Sustainability can be further improved by reducing overdiagnosis, unnecessary tests and interventions, the expert suggested: ‘The greenest scan is the one you don’t need to do.’ This mindset reduces emissions from the energy required by the scanner itself but may also avoid additional patient travel – another major source of healthcare-related GHG emission.
Recommended article
Article • Energy conservation & waste reduction
Reducing the eco-footprint of radiology
Contrast agents in the wastewater and power-hungry imaging systems: The eco-footprint of healthcare is huge, and radiology departments are among the main culprits. An expert panel at the ECR Overture explored ways to make the field “greener”.
Know thy waste management
Another area with huge potential for improvement is waste management, Dr Sheard said, pointing out how incorrect disposal of consumables can greatly enlarge any procedure’s carbon footprint. For example, contrast bottles, tubing sets and residual contrast are often indiscriminately thrown into the bin for sharps and infectious waste, she reported. This type of waste is incinerated – a highly carbon-intensive procedure that generates 1.85 tonnes of CO2 for every tonne of waste. ‘Often, only a very small part of the equipment – for example, the spike used for injection – needs to go into the sharps bin. All of the plastic tubing can be thrown into the non-infectious/offensive waste stream.’ This mode of disposal even has a negative carbon footprint, using the excess heat from burning other waste to generate the required power. Leftover contrast agent can be collected in a special tub and sent to the supplier for proper disposal, while the rinsed contrast bottles are perfectly fine to go into regular municipal recycling.

Image source: Adobe Stock/BillionPhotos.com
While acknowledging that the complexity of clinical waste disposal can be quite off-putting, the expert urged that staff must be educated on this topic: ‘Often, people just lack confidence to separate things, and are worried about risking contaminating waste streams by putting the wrong thing in there. Therefore, they take the safest street, which is to put everything into the highest clinical hazard category. Much more clear instruction is needed here, as this can make a huge impact.’ In a radiology ward with two CT scanners, where this approach was put into practice, Dr Sheard reported that the amount of waste disposed in the sharps/infectious bin was reduced by 98%, saving € 11,300 and over 20,000 kg of CO2 equivalents per year.
In conclusion, Dr Sheard pointed out that there are many more ways to reduce the carbon footprint of radiology – for example, by using renewable energy sources, or buying imaging systems according to their environmental impact. However, the most important factor as well as arguably the biggest challenge is behavioural change, she appealed to her colleagues: ‘Anything you can do to normalise sustainable healthcare, to start the discussion in your department and empower the people around you, is going to be very valuable. Finally, get a team together, network, and use your position as clinician to bother the chief executives, to put this issue on their agenda.’
References:
- Chua et al.: The Environmental Impact of Interventional Radiology: An Evaluation of Greenhouse Gas Emissions from an Academic Interventional Radiology Practice; Journal of Vascular and Interventional Radiology 2021
- McAlister et al.: The carbon footprint of hospital diagnostic imaging in Australia; Lancet Regional Health – Western Pacific 2022
29.03.2023





