Sponsored • Respiratory support
Extracorporeal technology eases stress
Conventional therapy for ARDS patients and for patients with exacerbation of chronic obstructive pulmonary disease (COPD) has relied on invasive mechanical ventilation. Mechanical ventilation, however, has several major drawbacks: sedation has to be induced and the air being pressed into the lungs with positive pressure can damage the pulmonary alveoli or the diaphragm. Moreover, even maximum ventilation frequently does not provide adequate gas exchange.
Innovative artificial lungs, which breathe for the patient, offer less traumatic treatment for severe diseases such as acute respiratory distress syndrome (ARDS) or chronic obstructive pulmonary disease (COPD)
2013, German firm Xenios AG was founded by the two medical device companies Novalung GmbH and Medos Medizintechnik AG. Its focus lays on developing and manufacturing innovative devices for minimally invasive lung and heart support and offering groundbreaking solutions for lung failure as well as surgical and interventional solutions for the treatment of heart disease.
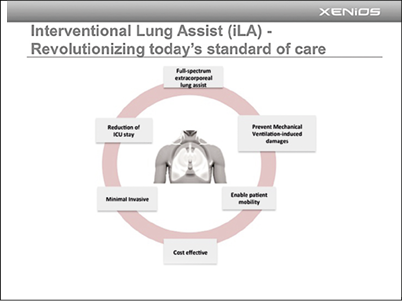
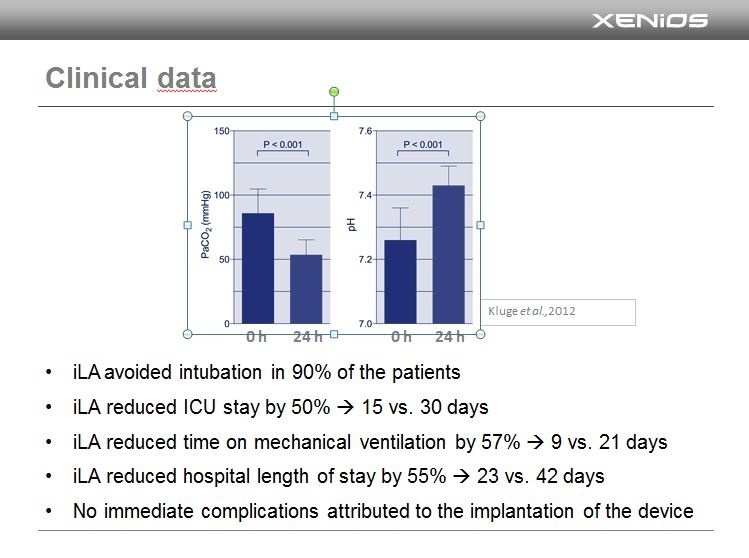
The Novalung product family is the first complete product range of state-of-the-art solutions for minimally invasive treatment of acute and chronic lung failure without mechanical ventilation and without the need for patient sedation and mobilization. XENiOS novalung products enable therapies for lung failure that are adapted to specific indications and patients. The duration and intensity of extrapulmonary lung support can be selected and adapted based on individual needs.
Thomas Bein, MD, University of Regensberg Medical Center:“Novalung’s lung support therapies can be dosed as required in order to individualize to a patient’s specific needs, which is a very significant clinical benefit.”
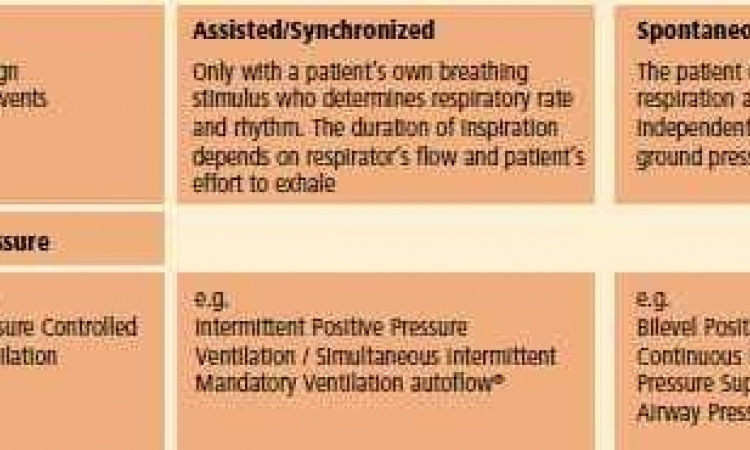
This new and easy-to-use alternative to invasive and trauma associated mechanical ventilation is usually comprised of a pump-driven pulmonary support system that removes carbon dioxide and adds oxygen. A key component of such a device is the so-called membrane ventilator, which ‘breathes’ outside the patient’s body to perform some of the gas exchange work of the native lung, at the same time relieving the respiratory muscles.
A plasma-tight diffusion membrane is connected femorally, for example, to the body via a vascular access. The blood pump can be adjusted precisely and instruments control blood flow. The membrane ventilator can be used on a patient for up to 29 days. Because the lung assist system does not require sedation, in that period the patient is actively involved in the therapy and can eat and communicate.
The hardware fits on a trolley, providing patient mobility during the therapy, the manufacturer adds. The membrane ventilator height can be adjusted quickly, for example, when the patient wants to lie down, sit up or be moved around. In addition, subsequent therapies can follow sooner, bringing length of stay reductions and thus reduced costs.
The next generation of lung assist systems might well be portable, the report continues. The platform-based technology enables further developments, such as smaller and other types of vascular access plus increased efficiency as state-of-the-art gas exchangers provide better performance with a smaller footprint. What might the far-off future bring? Perhaps bio-hybrid systems that mimic nature and are even colonised with cells.
Source: Xenios AG
06.06.2016