Article • Enzyme extended-spectrum beta-lactimase
ESBL: A greater danger than MRSA?
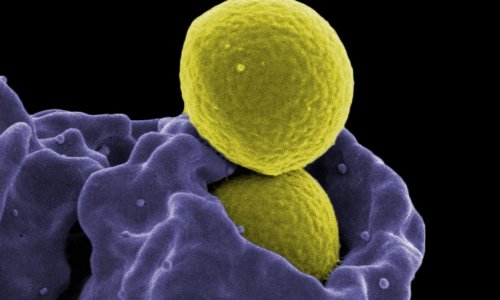
In hospitals, MRSA is considered Public Enemy Nr 1, and the increase in nosocomial infections, worldwide, has drawn universal attention to this ‘superbug’. However, Staphylococcus aureus is not alone:
Report: Karoline Laarmann
Credit: Aktion Meditech
Other pathogens are proving their resistance to antibiotics, in the last decade, gram-negative enterobacteria, which form the enzyme extended-spectrum beta-lactimases (ESBL), have joined the nasty high flyers. Produced by some bacteria, these enzymes even destroy the antibiotics effective against MRSA. Professor Christian Ruef, head of Hospital Hygiene at the Clinic for Infectious Diseases and Hospital Hygiene, University Hospital Zurich, Switzerland, has even forecast a shift of prevalence.

‘MRSA will never disappear completely,’ says Professor Christian Ruef, ‘but ESBL will cause us many problems in various European countries as well as in the USA, Australia and Japan, where enhanced resistance is already more widespread.’ As with MRSA, the reasons for multi-resistance are mainly the overuse of antibiotics, along with insufficient hygiene management, particularly hand disinfection. The situation is worsened by the fact that ESBL-producing pathogens are much more prevalent (community-acquired) than MRSA. In addition, as with MRSA, a geographical, north-south divide is distinguishable.
In an international comparison, the MRSA situation in Switzerland is relatively stable. With a rate of 5% the prevalence is similarly as low as in Scandinavia and the Netherlands. ‘I don’t believe that our prevalence figures are good because our hygiene standards are better than those of our neighbours, Germany and France, for instance,’ Prof. Ruef points out. ‘In fact, I think that we in Switzerland have simply been spared, so far. It’s always easier to maintain a low rate of occurrence than to lower a high rate. However, at University Hospital Zurich the development shows that, in the last two years, we’ve had twice as many ESBL cases than MRSA cases (120:60), unfortunately with an increasing trend.’
Similar to MRSA, enterobacteria are part of the normal bacterial flora of humans, although restricted to the intestine. However, if they spread from there they can lead to respiratory and urinary tract infections, postoperative wound infections and septicaemia (systemic infection). As ESBL pathogens are transferred, just like MRSA, by hand contact, but also through surface contact, they require the same hygiene and isolation procedures as MRSA infections.
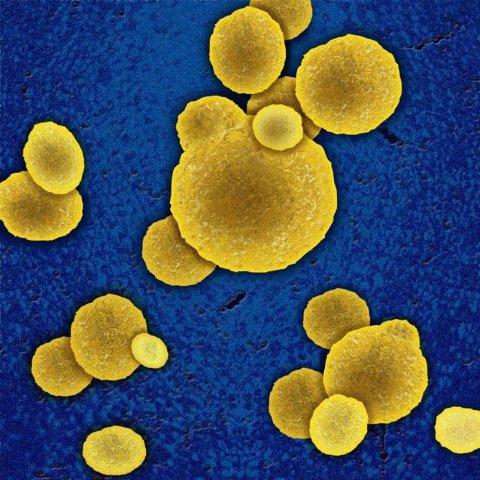
What specific dangers do ESBL producing bacteria present? ‘Bacteria of the family enterobacteriaceae, such as Escherichia coli and Klebsiella pneumoniae, which produce extended-spectrum beta-lactimase, are basically no more dangerous than multi-resistant Staphylococcus aureus, with the exception of risk groups such as older patients, where ESBL pathogens can lead to severe infections faster. The difficulty is that ESBL producing, gram-negative bacteria can inactivate almost all beta lactim antibiotics that are effective in the case of MRSA infection. This means that many ESBL carriers are not only resistant to Cephalosporin but also to antibiotics such as Chinolon. Very often this means that oral treatment is not an option. Outside the hospital the reserve antibiotics cannot be used against ESBL infections because they can only be given in the form of injections or infusions due to their increased toxicity.’
This year, the University Hospital Zurich has experienced a particularly unusual wave of infections with a further pathogen with problem resistance: 20 cases of Vancomycin-resistant enterococcus (VRE) occurred. ‘VRE was previously never a problem in our hospital, which is why this occurrence should be viewed as an epidemiological outbreak,’ Prof. Ruef explained.
The transfer of VRE strains from animals to humans has been largely contained through an EU-wide ban on the use of antibiotics in factory farming. For a long time, VRE was therefore all but forgotten. Meanwhile, VRE outbreaks are now occurring more frequently as regionally limited clusters in cities or certain hospitals. Similar to MRSA and ESBL, the treatment spectrum is severely limited. Linezolid is an antibiotic that makes oral VRE treatment possible, as an alternative to intravenous therapy, but this medication is very expensive.
In the future, Prof. Ruef sees a particular problem in the complete resistance of some pathogens. With MRSA and ESBL, as yet this is luckily not the case, he believes. ‘There are other examples, such as Acinetobacter, where this broad or complete resistance occurs again and again, and therefore endangers patients’ lives enormously. That’s why we need to improve the early detection and resistance determination as well as the development of new antibiotics.’
07.07.2010