© thatinchan – stock.adobe.com
News • Discussion on nomenclature
“Prostate cancer” or “incidentaloma”: What should early findings be called?
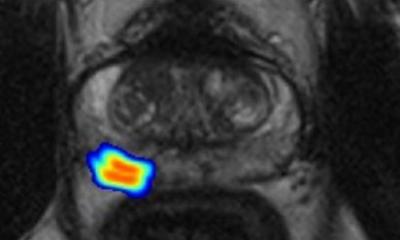
Prostate cancer is the second leading cause of cancer death worldwide in men, but far more patients are diagnosed than die of the disease.
In 2022, there were nearly 1.5 million cases of prostate cancer, but only 400,000 deaths. Low-grade prostate cancer, commonly known as GG1 among physicians, virtually never metastasizes or causes symptoms. Some medical researchers have wondered recently if it would be a benefit to public health to call GG1 something other than cancer.
To further this discussion, researchers convened an international symposium with participants from multiple fields, including patient advocacy. From this comes a new paper in the Journal of the National Cancer Institute, published by Oxford University Press, which indicates that patients may benefit if doctors stop calling certain early-stage changes to the prostate “cancer” at all. Key considerations included the very high rate of GG1 detectable on autopsy studies, the focus of contemporary diagnostic tests on detecting higher grade cancers, the benefits of relegating GG1 to something more like “incidentaloma” status, the adverse health effects of overtreatment, and the psychological burden of a cancer diagnosis for patients.
We absolutely need to monitor these abnormalities no matter what we label them, but patients should not be burdened with a cancer diagnosis if what we see has zero capacity to spread or to kill
Matthew Cooperberg
Those who convened at the meeting emphasized that while GG1is common among older men, it should not be considered normal. Patients with this condition should continue to monitor it with their physicians, according to investigators.
One concern is that patients may not bother to monitor the progression of the condition if their doctor doesn’t use the word “cancer” to explain what’s going on. Ultimately, those involved in the discussion emphasized, the goal of prostate cancer screening, diagnosis, and treatment is to bring down mortality rates while also reducing the harms of overdiagnosis and overtreatment. Matthew Cooperberg, the principal investigator involved with the symposium, believes that a reconsideration of nomenclature may be a good way to help bring this about.
“The word ‘cancer’ has resonated with patients for millennia as a condition associated with metastasis and mortality,” explained Cooperberg. “We are now finding exceptionally common cellular changes in the prostate that in some cases presage development of aggressive cancer but in most do not. We absolutely need to monitor these abnormalities no matter what we label them, but patients should not be burdened with a cancer diagnosis if what we see has zero capacity to spread or to kill.”
Source: Oxford University Press USA / Journal of the National Cancer Institute
01.10.2024