Article • Lab medicine in the Netherlands
Digital pathology: From over-promising to a reality check
Almost five years ago, the plan to implement a wide-ranging digital pathology approach across the Netherlands began to take shape. As more labs across the country acquire digital pathology capability, with steps to create a strong and accessible image repository and a national image exchange platform, one of the project leaders, Professor Katrien Grünberg, offered an update and spoke of some challenges that still lie ahead.
Report: Mark Nicholls

Almost five years ago, the plan to implement a wide-ranging digital pathology approach across the Netherlands began to take shape. As more labs across the country acquire digital pathology capability, with steps to create a strong and accessible image repository and a national image exchange platform, one of the project leaders, Professor Katrien Grünberg, offered an update and spoke of some challenges that still lie ahead.
In a keynote presentation, ‘Digital Pathology going Dutch’ at the recent Digital Pathology and AI Congress in London, she also touched on the experience in Nijmegen, where she is Professor of Pathology and chair of the Department of Pathology at Radboud University Medical Centre (UMC). ‘Sometimes we over-promise and sometimes we have to have a reality check,’ Grünberg told delegates as she outlined the healthcare landscape in the Netherlands regarding pathology with 90 hospitals, 50 pathology departments with 350 pathologists and 27 molecular facilities. Of the 50 labs, 16 had scanners in 2017, increasing to 23 this year, leaving 27 labs still without scanners, Grünberg pointed out.
Key trends and challenges
Key trends in the country are more molecular diagnostics; digital pathology and AI; and increased scale as well as a move towards specialising. All these trends are ‘game-changers’ by themselves, she said, but in addition, they interact too. Whilst Radbound UMC has a strong reputation for computational pathology, she acknowledged bringing it into everyday practice has not always proved straightforward.
Grünberg outlined how, four years ago, Radboud made the decision to move to digital pathology, wishing to start the roll-out in 2019. ‘We had hoped to have our first algorithms into practice in 2020, but that is now more realistically going to be 2021,’ she continued. ‘While digitising is all connected to machines, on the people side the technicians and pathologists have been very active in redesigning the workflow and integrating digital pathology into a highly-tuned laboratory workflow. They are right in the middle of living through the transformation process. It’s hard work and requires perseverance and endurance and you have to believe that, in the end, it will revolutionise your work. While you keep going you also still have to provide a quality and efficient service for patients.’
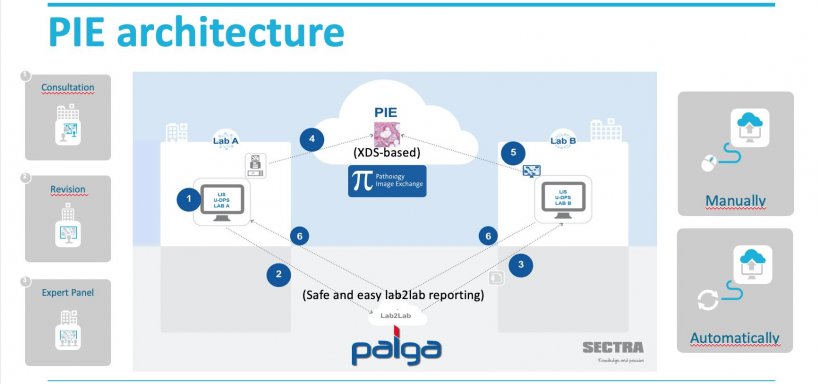
A core component of the march towards digital pathology in the Netherlands has been to establish a Pathology Image Exchange (PIE) at a time of more lateralisation in the country’s healthcare, with patients being treated in different locations and often closer to home.
From pathology focus groups, an aspect that emerged was that whole slide imaging was the way to go to build the national imaging platform. ‘The requirement to be vendor neutral was key,’ said Professor Grünberg. ‘We had to make it available to all pathology departments in the Netherlands.’ She explained the PIE architecture was designed with the direction of flow of images and reports taking different routes to come together at the receiving end and also a manual and automatic workflow, for high volume of consultation.
Recommended article

Article • Linked laboratories
New Dutch digital pathology advances
Efforts have been made to digitise pathology in the Netherlands, where the Dutch pathology network PALGA has run since 1990, connecting all of the Netherlands’ laboratories. Paul J van Diest, head of the pathology department at the Utrecht University Medical Centre, presented the brand new Dutch digital pathology platform during ECP 2018. Launched this year, this enables quicker, easier…
Work in progress
Although moving forward, the project is still ‘a work in progress’, Grünberg pointed out. It remains costly and complex for labs to link and, at this stage, only seven labs are connected to the PIE at a time of rapid market developments and increasing costs. In addition, DICOM standard is not as standardised as hoped with a ‘to do’ list that still includes a drive to connect labs to PIE and implement Lab2Lab connectivity, tackle DICOM issues and costs.
Artificial intelligence (AI) has an important role to play, with deep learning a powerful tool with computer aided quantification and grading, with AI eventually becoming an integral part of the overall assessment process. One of the big challenges for the computational group was in getting good data sets to lead to good algorithms. ‘A good way to do that is to team up with other hospitals to build up a really good archive,’ Grünberg continued. ‘You have to team up to create a large repository, especially for rare diseases.’
The dream is for a flexible data repository within the platform where participants can contribute and access data and while secure data storage has not been a major problem, she conceded there have been challenges around secure data transfer. Yet at Radboud, and across the Netherlands, there remains a determination to rise to the challenges of promoting AI development by organising access to data.
Profile:
Katrien Grünberg is Professor of Pathology and chairs the Department of Pathology at Radboud University Medical Centre in Nijmegen, the Netherlands. She is also Past President and current board member of the Dutch Society of Pathology.
11.05.2020