Article • Distinguishing arteriopathies
Deterring paediatric acute stroke
Acute stroke in children has the same incidence as brain tumours and can seriously affect a patient’s life. Two kinds of arteriopathies are common drivers of paediatric acute stroke and radiologists must learn to distinguish their signs as early as possible to improve prognosis, according to Béatrice Husson, a paediatric radiologist at Le Kremlin Bicêtre Hospital in Paris.
Report: Mélisande Rouger

‘Acute stroke can trigger focal motor deficit in so-far healthy children. There can be diagnostic wandering because deficit, before being definitive, can regress and fluctuate for many hours or even days, and because knowledge of this ischemic aetiology is still insufficient and wrongly attributes diagnosis to migraine or epileptic seizures with Todd’s paresis,’ said Husson at the recent JFR, the French Society of Radiology’s annual meeting, online.
Unlike adults, a leading cause of acute stroke in children is arteriopathy, especially focal cerebral arteriopathy, which causes 30 to 40% of paediatric strokes, with unilateral damage of anterior circulation, and vertebral arteriopathy, a less common yet typical condition of the paediatric age. ‘The first thing to remember when imaging a child with suspected stroke is to avoid using sedation, which could complicate patient neurological monitoring and is no longer necessary given the important reduction of acquisition times in MRI,’ she advised.
Tending to the child in a calm and comforting atmosphere without losing time is paramount. MRI is the first choice modality in these patients, except when they present with consciousness disorders. “In this case,’ Husson added, ‘we’ll carry out a CT scan with an anaesthetist resuscitator at our side.’
MRI protocol includes a diffusion sequence, T2 or magnetic susceptibility sequence, FLAIR axial study, TOF MRA at the level of the circle of Willis, MRA of cervical arteries, non-contrast perfusion – if possible – and a T1 sequence. For CT, radiologists should perform non-contrast head CT, followed by arterial CT angiogram of the head and neck.
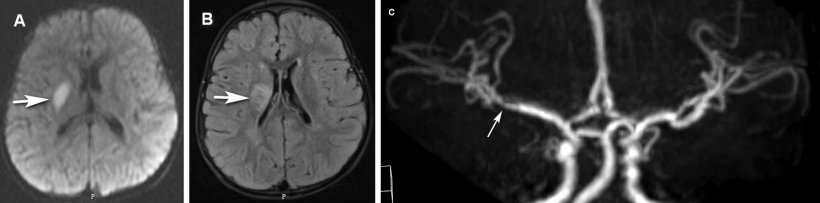
Figure A: axial diffusion sequence. Hypersignal of the right lenticular nucleus (arrow) linked to acute stroke in deep right MCA
Figure B: Flair T2 sequence. Hypersignal of the right lenticular nucleus (arrow) confirming constituted stroke four hours earlier
Figure C: Face reconstruction of the Willis polygon (acquisition with a TOF MRA sequence), showing distal stenosis of the M1 segment in the right MCA (arrow)
Husson shared several clinical cases with the audience, including the images of a child presenting with deep left ischemic stroke and occlusion of the left middle cerebral artery. Thrombectomy was initiated and recanalization looked satisfying on angiographic images before and right after procedure, however following MRI showed renewed occlusion and stroke extension a few hours later. ‘This evolution, and these possible complications, can be explained by the aetiology of this focal brain arteriopathy, which we believe is linked to arterial wall inflammatory damage that may be caused by infection. The most common infectious agents are varicella and zona viruses, and so we will systematically look for varicella infection 12 months before stroke in a child presenting with such symptoms, ‘ Husson explained.
MRI follow-up was able to show recovery and stabilisation of arterial lesions, enabling an end to antiplatelet treatment 18 to 24 months after the event. The second arteriopathy radiologists should suspect in children with acute stroke is vertebral arteriopathy. In this setting, stroke typically occurs in the posterior circulation with multiple parenchymal lesions in 40% of cases that are associated with localised arterial lesions in segments V2 and V3. ‘From this pathological area in the vertebral artery, embolus may cause basilar or posterior cerebral artery thrombosis,’ she said.
Recommended article

Article • PRIMAGE project
Aiming AI at lethal paediatric tumours
La Fe University and Polytechnic Hospital in Valencia, Spain, is coordinating EU-funded program PRIMAGE, which uses precision information from medical imaging to advance knowledge of the most lethal paediatric tumours, by establishing their prognosis and expected treatment response using radiomics, imaging biomarkers and artificial intelligence (AI).
To properly explore this arteriopathy, radiologists should perform additional, thin-sliced T1 SAT cervical sequence to look for wall haematoma because dissection must be suspected.
In addition to MRA at the level of the circle of Willis, it is mandatory to perform high quality cervical MRA, Husson explained. ‘I would recommend carrying out non-injected, cervical-centred TOF rather than injected SAT, which may prove complicated due to patient movement triggered by the injection, the combination of venous and arterial time and wide field study, which is not adapted to children’s small-sized vertebral arteries. If cervical MRA fails, then we’d be looking at an angio CT at arterial time. When none of these examinations help reach diagnosis, we may consider performing conventional angiography,’ she said.
A major risk of vertebral arteriopathy is recurrence, which is five times higher than in focal cerebral arteriopathy. Recurrence mainly occurs in the first three months after stroke and justifies anticoagulant treatment. In conclusion, one must remember high incidence of arteriopathy causing acute paediatric stroke. ‘Recanalisation treatment for unilateral focal arteriopathy with middle cerebral artery stroke and transitory inflammation at carotid T level can be discussed case by case. Recurrence may occur and justifies monitoring. After arterial stabilisation that is confirmed by MRI, antiplatelet treatment can be interrupted. The other arteriopathy radiologists must suspect is vertebral arteriopathy, which justifies maximal examination of vertebral arteries because this typical lesion affecting the segments V2 and V3 is highly suspicious of embolus that can cause basilar occlusion. ‘This finding,’ she concluded, ‘justifies thrombectomy whenever technically possible, and frequent early recurrence justifies initial anticoagulant treatment in children.’
Profile:
Béatrice Husson is a paediatric radiologist at le Kremlin Bicêtre Hospital (Groupe Hospitalier APHP Université Paris Saclay) in Paris, France. Throughout her career she has specialised in paediatric neurovascular malformation pathologies and rare paediatric brain inflammatory disease. Since 2013 she has been a referring radiologist for the National Referring Centre for Vascular Stroke in Children led by Dr Manoëlle Kossorotoff
01.12.2020