Article • Carbapenemase producing enterobacteriaceae
Detecting drug-resistant CPE quickly is still a challenge
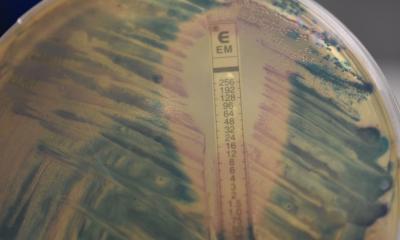
Early detection and confirmation of carbapenemase-producing enterobacteriaceae (CPE) are essential when choosing the appropriate antimicrobial therapy and to implement infection control measures. Here a leading Spanish microbiologist reviews an arsenal of tools currently available to clinicians.
Report: Mélisande Rouger
Resistance to beta-lactam antibiotics in enterobacteriaceae (EBc) is due to one or more of these mechanisms: drug inactivation by hydrolysing enzymes (beta-lactamases), the most common decreased permeability due to down-regulation of porin synthesis, up-regulation of efflux pumps and, less frequently, by target modifications. In particular, EBc resistant to carbapenemic agents, especially those producing carbapenemases, represent a public health concern, according to David Navarro Ortega, a professor of Microbiology at the Valencia School of Medicine speaking during the 10th Infectious Diseases Day that unfolded last March in Madrid.
Recommended article

News • Enigmatic enzyme
How bacteria recover from antibiotics exposure
Beta-lactam antibiotics, including penicillin, are one of the most widely used classes of antibiotics in the world. Though they’ve been in use since the 1940s, scientists still don’t fully understand what happens when this class of drugs encounters bacteria. Now, researchers at the University of Notre Dame have elucidated how an enzyme helps bacteria rebound from damage inflicted by…
The transmissible carbapenemases are divided into three different classes: class A (serine carbapenemases), class B (metallo-β-lactamases) and class D (OXA carbapenemases, such as OXA-48). Accurate detection of carbapenemase-producing enterobacteriaceae (CPE) constitutes a major laboratory diagnostic challenge. ‘In addition, we cannot reproduce faithfully in vitro what occurs within the source of infection,’ Navarro pointed out. ‘This remains one of our main obstacles right now.’
Differentiation and prediction still take too long
The conventional algorithm to detect and distinguish among these classes of carbapenemases is too slow, up to 48 hours, the microbiologist explained. ‘We check if the bacteria shows reduced susceptibility to carbapenems in routine inhibitory-based antimicrobial susceptibility testing (AST). If the test is conclusive,’ he said, ‘it‘s followed by a confirmatory test, and, optionally, genotypic characterisation.’
Spain follows the European committee guidelines on antimicrobial susceptibility testing (EUCAST) to detect resistance mechanisms and specific resistances of clinical and/or epidemiological importance. But the EUCAST meropenem screening criteria has been shown to have difficulties in detecting OXA-48 producers.
The “molecular antibiogram” is an interesting approach to detect EBs resistance to beta-lactam agents, but they predict resistance rather than susceptibility
David Navarro Ortega
A bunch of phenotypic confirmatory tests to detect carbapenemases are currently available, including combined-disk tests using specific inhibitors, such as EDTA and boronic acid, and the modified Hodge test (MHT).
A number of rapid phenotypic methods to detect carbapenem resistance mediated by carbapenemases, which can be completed in under two hours, have been described, including the detection of carbapenem inactivation by mass spectrometry (MALDI-TOF MS) or carbapenem hydrolysis by biochemical (Carba NP test or CarbaNP II TEST), or electrochemical methods (BYG Carba Test). These tests can be run either using cultured bacteria or bacterial pellets directly derived from clinical specimens, e.g. blood and/or urine.
‘The “molecular antibiogram” is an interesting approach to detect EBs resistance to beta-lactam agents, but they predict resistance rather than susceptibility. The latter could be obtained using genotypic, immunologic or mass spectrometry methods could, but they can only be seen as add-on methods to conventional AST testing,’ Navarro pointed out.
In the future, he concluded, analysis of bacterial pan-genomic sequences by sophisticated bio-informatic tools obtained by modern deep sequencing methods will provide clinically relevant data not only on bacterial resistance to antibiotics but also on bacterial pathogenetic traits.
Profile:
In 1985 David Navarro Ortega graduated in medicine at the University of Valencia (Spain), gained his medical doctorate in microbiology and immunology there four years later and became postdoctoral research associate at Lenore Pereira’s laboratory, University of California San Francisco (UCSF) up to 1991. He is now Full Professor of Microbiology in School of Medicine of Valencia and Head of the Microbiology Service at the Clinic University Hospital, Valencia. His research mainly concerns diagnostic, clinical, biological and pathogenesis aspects of herpes virus infections, especially cytomegalovirus in allogeneic stem-cell and solid organ transplant recipients, and in cases of inflammatory diseases and critically ill patients with no canonical immunosuppression. He has authored/co-authored over 260 publications in intermediate-highly- ranked journals and is a member of the Editorial Board of Diagnostic Microbiology and Infectious Diseases, a member of the ECIL group of the European Bone Marrow Transplantation Society (EBMT) and a regular reviewer for about 25 journals.
13.04.2019