Article • CAD pros and cons
CT or MRI – which is better for imaging stable cardiac chest pain?
When it comes to imaging stable cardiac chest pain, which modality should be used as the first-line test to investigate coronary artery disease: CT or MRI? Radiologists discussed the strengths and limitations of the two approaches in a lively Pros and Cons session at ECR Overture.
Report: Mélisande Rouger

Image source: Universitätsklinikum Freiburg
Initial assessment of patients with stable coronary artery disease (CAD) can be a bit of a head scratcher for radiologists. While MRI has proved its efficacy time and time again, new techniques and evidence suggest that CT is an equally viable, if not better tool to evaluate CAD right from the start of patient management, according to Prof. Fabian Bamberg, from Freiburg, Germany. ‘Traditionally, functional imaging has been overwhelmingly convincing,’ he said. ‘But with the recent advances and the evidence that’s available today, there’s only one way to go and it’s cardiac CT.’
The case for CT
CT presents with a long list of benefits: it’s a robust and reproducible technique that can be performed in just 3-5 minutes – which is a lot quicker than an MR scan, which takes at least 30 minutes. Furthermore, CT is more accessible to more patients, including those with medical implants, prosthesis, or claustrophobia. With the development of dose reduction software in the past decade, radiation exposure has decreased significantly. ‘This is not an issue anymore, so CT has very low side effects,’ Bamberg said.
Evidence that CT allows for at least non-inferior management of stable chest pain has been piling up. ‘There’s a whole bunch of studies that show that functional assessment is not superior to morphological assessment,’ the expert said. ‘So, for the majority of patients, it doesn’t make a difference whether you do functional or morphological imaging. As a baseline test, you have sufficient information to make similar decisions with similar outcomes if you rely on morphological assessment.’
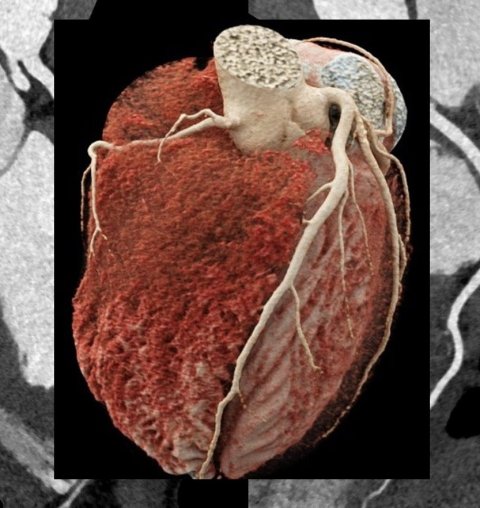
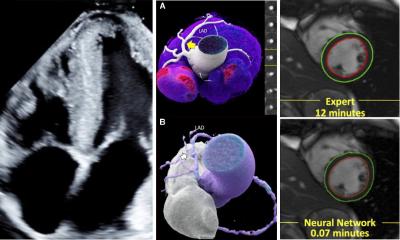
Image source: Prof. Bamberg
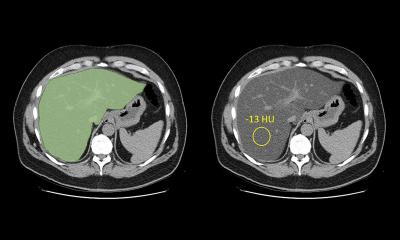
Thanks to new image post-processing software and AI, CT also offers more available information that physicians can use to improve patient prognosis and risk assessment – not just for the heart, but also other organs. ‘We can evaluate not just the arteries and plaque, but also diseases of the myocardium and outside the heart, for example lung cancer, osteoporosis and even breast cancer.’ CT provides incremental information that can be used to classify plaque burden, perform coronary classification, and assess functional relevance of morphologic changes.
The development of perfusion and CT functional flow reserve (FFR) techniques has enabled acquisition of anatomical and functional imaging in just one scan, with similar efficiency to MR. ‘For the majority of patients, cardiac CT is sufficient to come up with good decision-making,’ Prof. Bamberg concluded, ‘but MR is a good way to go when you need more information of the myocardium.’
Image source: Universitätsspital Zürich
CT is an ideal tool in many settings, Prof. Robert Manka from Zürich, Switzerland, said in the following talk. However, he conceded that there are still too many drawbacks to use it as a baseline tool for CAD. ‘Radiation dose remains high and neither CT FFR nor CT perfusion are recommended in the European Guidelines as first line methods for CAD assessment,’ he said.
The case for MRI
It’s extremely difficult to judge CAD by eyeballing alone, because many factors must be taken into account to make the correct diagnosis, Manka explained. ‘People are often not aware of it and think it’s about the stenosis degree, but it’s more about the complexity of the stenosis.’ MRI certainly takes longer than CT, but it enables to see the function behind the stenosis and get a bigger picture of what is going on. ‘On CT, you just look at the stenosis and you can also do quantification using software, but it will only show the degree of the stenosis and it doesn’t really help you know whether it’s relevant or not.’
CT is a perfect test if the patient has no stenosis at all – for example in a 40-year-old woman with atypical chest pain –, but not when the patient presents with vessel irregularities or stenosis. ‘You won’t be able to know if those findings are relevant or not because CT doesn’t show if they cause ischaemia to the heart,’ Manka said. ‘If something is not 100% normal, we have to do the test again.’
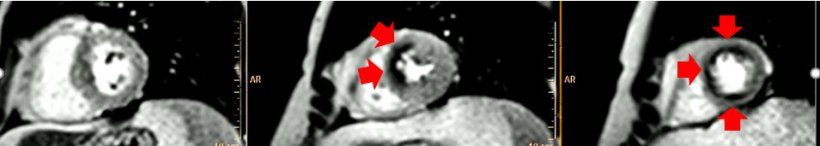
Image source: Prof. Manka
Research has showed that assessing the function of the vessel is linked with better patient outcomes. With MRI as a first-line tool, patients can be referred directly to coronary angiography, if necessary. ‘You can examine a broader range of patients: those with a low pre-test probability and patients with a high pre-test probability. CT is rather for those with a low pre-test probability,’ the expert said.
The main issue is that many radiologists are not aware of the pros and cons of the method. ‘You’d tend to believe that you can do a CT scan to exclude stable CAD in 70-year-old patient – but this is wrong because those patients already have a lot of calcium and it will be difficult to exclude the disease with CT,’ Manka said.
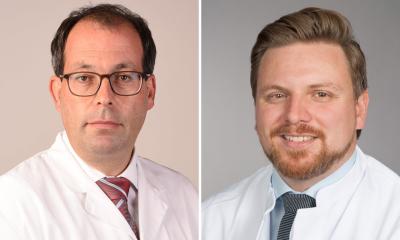
Profiles:
Professor Fabian Bamberg is chair of radiology at the department of diagnostic and interventional radiology at the University of Freiburg, Germany. He received his medical degree from the University of Witten-Herdecke and graduated with a masters’ degree in public health from Harvard School of Public Health in 2007. He served as a faculty member in the Cardiac MR PET CT Program at Massachusetts General Hospital, Harvard Medical School, Boston, USA, and then joined the department of radiology in Munich in 2008. There, he completed his fellowship at the Ludwig-Maximilians University and directed the MRI program as an attending physician. His research focuses on the assessment of new imaging technologies in a clinical and epidemiological context, with a special emphasis on diagnostic accuracy, impact on clinical decision-making and cost-effectiveness. He has received many research prizes and he sits on the editorial board of the Journal of Cardiovascular CT and Journal of Thoracic Imaging. He is one of the main investigators of the German National Cohort MRI Study, a large population-based whole-body imaging trial.
Professor Robert Manka is the director of the cardiac magnetic resonance imaging unit of the University Hospital Zürich, Switzerland. He was trained at the University of Bonn, the German Heart Institute Berlin and the University Hospital Zürich. He completed a postdoctoral fellowship at the Institute for Biomedical Engineering at the University and ETH Zürich. His research focuses on developing cardiovascular magnetic resonance imaging methods, specifically for the assessment of ischaemic heart disease and heart failure. In 2013, he received the Venia legendi (Habilitation) from the University of Zürich. Professor Manka is an ESC CMR Exam Board member, Chair for CMR Laboratory Accreditation and a member of the SCMR Clinical Practice Committee.
04.03.2022