Article • Coronavirus imaging
Covid-19: Is CT more sensitive than PCR testing?
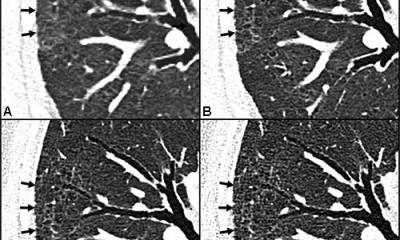
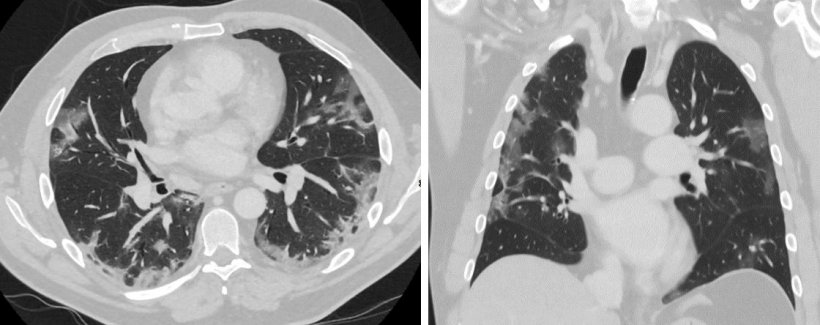
Covid-19 causes characteristic changes in lung tissue visible in CT scans and chest radiographs. The “ground-glass” opacities are sharply delineated areas, bilateral and mainly located in the basal and peripheral lung sections.
Report: Michael Krassnitzer

In the course of the infection, the opacities become increasingly consolidated. In the first wave of the Covid-19 pandemic, when PCR tests (RT-PCR) were scarce and had high turn-around-times and when many suspicious cases had to be assessed, CT was sometimes used for diagnostic purposes. Initially, publications from China even considered CT to be superior to RT-PCR. ‘This sparked an international debate among radiologists and clinicians about the role of CT in the diagnostic work-up of Covid-19,’ said Professor Cornelia Schäfer-Prokop, radiologist at Meander Medical Centre in Amersfoort, the Netherlands.
Today, RT-PCR is considered the gold standard. ‘However, it’s a suboptimal gold standard,’ the professor added, during a presentation at the Vienna Radiology Symposium (5-7 November 2020). In a PCR test, viral RNA is converted into DNA with the help of the enzyme reverse transcriptase (RT) and then examined using polymerase chain reaction. Its major advantage is high specificity. Negative test results are almost 100 percent correct, i.e. false positives are extremely rare. The test’s problem is its low sensitivity: the literature, according to Schäfer-Prokop, mentions 60-70%. Many factors affect sensitivity, such as the duration of symptoms, quality of the sample and the assay used or viral load when the test was performed. Thus, an RT-PCR test might have to be repeated several times, particularly when clinical suspicion is high but the test results are negative.
Recommended article

Interview • Chest X-ray, CT and more
Imaging the coronavirus disease COVID-19
Chest X-ray is the first imaging method to diagnose COVID-19 coronavirus infection in Spain, but in the light of new evidence this may change soon, according to Milagros Martí de Gracia, Vice President of the Spanish Society of Radiology (SERAM) and head of the emergency radiology unit at La Paz Hospital in Madrid, one of the hot spots for viral re-production of COVID-19.
By contrast, CT sensitivity is considered to be above 90%. In other words: in at least 90 of 100 infected people the infection will be detected. That sounds good, but can be a problem when the disease is not widespread. ‘With a prevalence of less than 10%, CT is not suited for screening or primary diagnosis, since potentially there will be too many false positives,’ she explained. Other viral infections can yield very similar CT findings, which is important above all in winter months. A cardiac oedema, or an acute form of interstitial fibrosis (NSIP), for example, are typical non-infectious mimics of Covid-19 – some patients present with fever and cough and, on the images, the lung tissue changes related to these conditions look very much like the changes caused by Covid-19.
Today, guidelines specify when CT is indicated in the Covid-19 context, e.g. the multinational consensus statement published by the Fleischner Society, an international and interdisciplinary society for thoracic diseases. Schäfer-Prokop listed the following criteria that indicate a CT:
- high probability of infection (typical symptoms, contact with infected persons) but negative initial RT-PCR
- comorbidities and thus increased risk of severe disease progression
- moderate and severe symptoms
- complications are suspected (pulmonary embolism, superinfection).
‘CT is not recommended routinely for screening people without symptoms or with mild discomfort, except when comorbidities are present,’ the German radiologist emphasised, adding: ‘As mentioned before, each positive finding should be confirmed by RT-PCR due to the potentially overlapping CT findings. ‘In the course of the pandemic, what I learnt is that we should evaluate the radiology images never by themselves but always in the clinical context,’ she confirmed.
Today, we know that coagulopathy is one of the most frequent complications, that means the risk of acute pulmonary embolism is increased by more than 30 percent
Cornelia Schäfer-Prokop
Typical clinical symptoms are dry, unproductive cough, fever, fatigue, loss of sense of smell and taste, shortness of breath. Additionally, there are typical lab findings such as high levels of C-reactive protein (CRP) and lactate dehydrogenase (LDH), elevated ferritin and D-dimer levels, as well as a pathological granulocyte to lymphocyte ratio. ‘Today, we know that coagulopathy is one of the most frequent complications, that means the risk of acute pulmonary embolism is increased by more than 30 percent.’ Sudden worsening of respiratory status, a high D-dimer baseline value and/or significantly elevated D-dimer levels, therapy-resistant hypoxaemia, tachycardia, hypotension and right ventricular load are frequent clinical indicators and, according to Schäfer-Prokop ‘a good reason to perform a contrast-enhanced CT’.
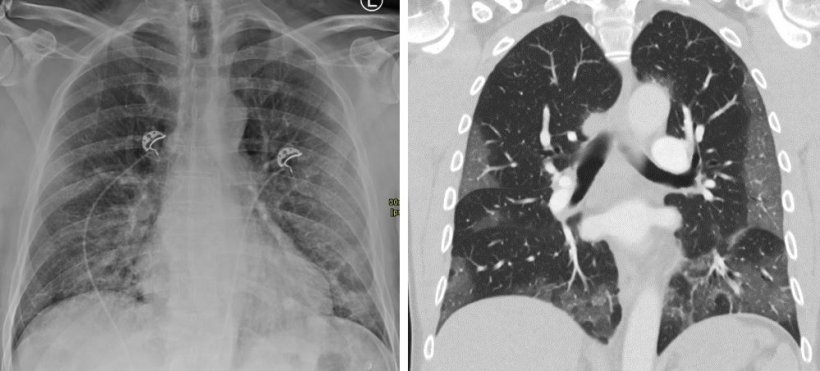
Imaging – be it radiography or CT – not only supports diagnosis but also has predictive value, the radiologist explained, pointing out results from four studies: the extent of changes in the lung tissues detected in chest X-ray correlates with hospital admission and intubation; clinical parameters combined with chest X-ray allow a prognosis regarding ICU admission and death; reduction of ventilated lung parenchyma detected in CT, combined with clinical parameters, correlates with ICU admission and death; radiomics and clinical parameters predict intensive care and death better than imaging, radiomics and clinical parameters alone.
Profile:
Professor Cornelia Schäfer-Prokop joined the Meander Medical Centre in Amersfoort, the Netherlands, in 2009. The radiologist also researches at the Department of Radiology and Nuclear Medicine at Radboud University Medical Centre in Nijmegen. From 1993-98 she was in Hanover and, from 1998 to 2004, at AKH Wien. Her work continued, between 2005 to 2009 at AMC Amsterdam. Her research focus is on digital radiography, computer-aided detection and classification, as well as diagnostics of interstitial lung disease. The professor has been a member of the Editorial Board of European Radiology, the Journal of Thoracic Imaging, Radiology and Insights into Imaging; she is also member of the Fleischner Society.
03.12.2020