Article • Corona consequences in Spain
COVID-19 fears put interventional cardiology on lockdown
The number of primary angioplasties – the main treatment for heart attack – has dropped by 40% in Spain since the beginning of the coronavirus lockdown.
Report: Mélisande Rouger
Other key diagnostic and therapeutic procedures have also considerably diminished. Spanish cardiologists are urging the population to call the emergency medical systems whenever symptoms of myocardial infarction occur, in spite of fears linked to the COVID-19 pandemic.
Significant reduction of interventional cardiology treatments
The COVID-19 pandemic and the following lockdown in Spain have triggered a drastic reduction in the number of interventional cardiology procedures carried out in the country, a study published by the Spanish Society of Cardiology and the Association of Interventional Cardiologists recently showed. A remote enquiry was carried out at 71 cardiology services across the 15 autonomous communities, to compare the activity over a week before the start of the pandemic (February 24 - March 1) with the activity during the first week of lockdown (March 16 - 22).
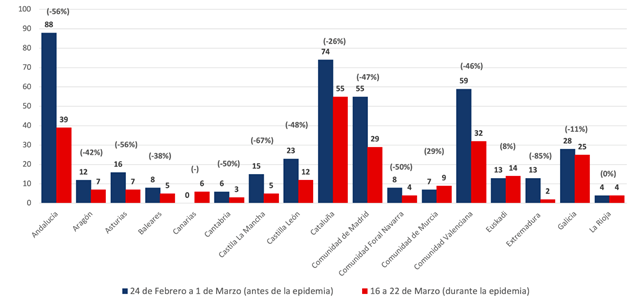
The authors found out that significantly fewer procedures had been carried after the beginning of lockdown, with 57% fewer diagnostic examinations, 48% fewer therapeutic coronary procedures and 81% fewer structural trans catheter procedures interventions. Primary angioplasties performed in acute myocardial infarctions also significantly diminished from 429 in the last week before the epidemic to 258 in the first week during the epidemic, i.e. a 40% reduction. The drop was observed all across the country but especially in Extremadura (-85%), Castille-La Mancha (-67%), Andalusia and Asturias (-56%).
Spanish cardiologists were anticipating these results and launched the study to confirm their doubts, according to Ángel Cequier, President of the Spanish Society of Cardiology and Professor of Cardiology in the University of Barcelona. “It was our perception when the pandemic started. We noticed that fewer patients with myocardial infarction were being transferred much less often, so we decided to carry on a study, which confirmed our suspicions,” he said.
Excessive delays threaten patient prognosis

Cardiologists agree that the main driver behind this dramatic drop is that patients are afraid of visiting the hospital and catch the virus. “We fear that many patients with low to moderate chest pain avoid going to the hospital or arrive with delay, because they are afraid of becoming infected,” he said. Another lesser cause for the reduction of cardiology activity may be that people with known or unknown cardiovascular disease are resting at home and avoid important physical exercise, which may reduce potential instability, Cequier added. The reduction in primary angioplasty activity is alarming, the authors noted, as this could lead to a posterior increase in cardiovascular mortality both in the short and long term.
Myocardial infarction (MI) causes more than 14,500 deaths per year, and it is vital for patient survival to receive early and optimal treatment. MI treatment consists in opening the blocked coronary artery as rapidly as possible using catheterization. “Any delay in receiving appropriate treatment produces progressive cellular death in the myocardium and increases the extension the myocardial infarction,” Cequier said. Delayed treatment can generate important complications in the long run as well, as the heart loses strength and the ability to contract itself, which can bring damage and death. “Not opening the artery as early as possible means that the infarction will affect an important part of the heart and it is associated with important complications,” he said.
Patients now arrive at the hospital with excessive delay – eight, ten or even twelve hours after the symptoms onset. Ideally the artery should be opened in the first six to eight hours to bring major benefits. After that window closes, and especially after twelve hours, the infarction is almost established, meaning that the treatment will not be that beneficial. If an artery that normally feeds the heart with oxygen and nutrients is blocked, the whole territory that is normally covered by this artery dies. “This part of the heart will not work and the heart will not move all the blood it needs.” he said.
The degree of uncertainty related with isolation and lockdown, for example work instability, can have an impact
Ángel R. Cequier Fillat
If anyone suffers sudden moderate to severe chest pain and that pain is accompanied by sweat, feeling unwell or pain in the left arm and/or the neck for more than 25 minutes, they should dial 112 right away. They will be dispatched to hospitals that offer dedicated treatment, following the Code Infarction in place in Spain. Cardiology and interventional cardiology services continue to offer the same quality service during the pandemic, Cequier insisted. “We are very well equipped and prepared. We are at full capacity, even with the midst of the pandemic.”
The organization of some cardiology departments had to be revised in areas particularly affected by the pandemic, such as Madrid or Catalonia. “We see more patients with COVID-19 than cardiovascular patients these days. Our team includes a majority of young cardiologists, as older colleagues are more at risk of catching the virus. We work in multidisciplinary teams with the full support of pulmonologists and internal medicine physicians,“ he said.
Recommended article

Article • The math behind corona
Predicting the future of the Covid-19 pandemic with data
Mathematical models can help shed light on the evolution of the coronavirus pandemic, according to Spanish mathematician Juan Luis Fernández Martínez, who predicted Spain could have between 90,000 and 160,000 infected patients. The next trend in epidemic data science will be to issue prediction models that focus on early detection.
COVID-19 complications increase mortality
More cardiovascular deaths are expected in the coming weeks due to the epidemic, as many hospitalized patients with COVID-19 present with cardiovascular complications. One such complication is myocardial infarction in patients with respiratory issues. About 25% of patients with COVID-19 who develop respiratory complications in the hospital develop myocardial lesions as well. These complications are more common among the elderly and fragile patients, who already have other risk factors, such as diabetes, hypertension.
Another aspect that will be interesting to see in a few weeks will be the effect of lockdown on cardiovascular health. “The degree of uncertainty related with isolation and lockdown, for example work instability, can have an impact. We could see more patients in the coming weeks, after the lockdown. The number of selected patients will certainly increase in the weeks to come,” he concluded.
Profile:
Dr. Ángel R. Cequier Fillat has been Director at Heart Disease Institute in the Bellvitge University Hospital in Barcelona (2010-2019). He is Professor of Cardiology at University of Barcelona and President of the Spanish Society of Cardiology. He was the Head of the Cardiovascular Group Research IDIBELL (Bellvitge Research Institute) and President of the Scientific Committee Acute Myocardial Infarction (AMI) Code in Catalonia.
06.04.2020