Computer-assisted coding
Every hospital does it, but how accurately and consistently coding is done has a major effect on the quality of treatment and also on the bottom line. Traditionally so-called ‘coders’ determine which code to apply for a specific medical service.‘
Report: Cornelia Wels-Maug
‘Pie in the sky?’
In the case of digital records, coders typically use software that enables them to key in a certain medical condition or treatment and then the software comes up with a selection of codes to choose from’, explained Markus Stein, Director Patient Management at the private Ethianum clinic in Heidelberg. Once the codes are assigned, a claim can be issued.
How accurate the billing is depends on a number of factors, but particularly on the completeness of the documentation, the legibility of records, the consistent application of coding rules, and the use of a harmonised medical terminology. The fact that the documentation is often done after a patient’s discharge does not help the accuracy of the process.
Volker Gertler, General Business Manager Western Europe of 3M Health Information Systems confirmed this: ‘Often coding is delayed and is only done ex post, in tandem with patient discharge; inevitably some procedures will not be documented.’ This negatively affects an institution’s profitability because not all rendered medical services can be charged.
Given that ‘in Germany, 17% of all statutory health insurance claims are investigated for their correctness’, Gertler explained, an institution has every incentive to get the documentation and coding right.
Computer-assisted coding
The growing adoption of electronic health records (EHR) facilitates a more automated processing of digitised patient data that can be applied, among other things, to coding as well as billing.
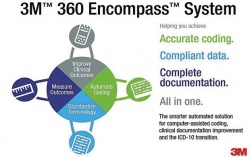
Computer-assisted coding (CAC) is software that scans medical records in the EHR, identifies key terminology as defined in the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT) and suggests codes for a particular procedure or service. Then a human coder reviews the codes.
CAC can also analyse the context of key words to determine whether they require coding. For example, the term ‘diabetes’ requires coding when it’s a diagnosis, but not when it is referring to a ‘family history of diabetes’. Additionally, CAC solutions can diagnose if a data source lacks information, e.g. in lab results, and will request the missing data.
CAC implementations are particularly driven by the transition to ICD-10 in the USA, which must take place by 1 October 2015. Hence, it was no surprise when Gertler explained that 3M developed a CAC solution, its KODIP Suite, first in the US, for the US market. ‘We have been selling it for the past two years, winning approximately 1,000 clients,’ he said.
However, with a lower EHR adoption in Europe, the current prospect of an uptake of CAC solutions is less compelling, as the investment into CAC will be much harder to leverage.
Stein reckons: ‘A fully automated coding process such as computer-assisted coding is still a pie in the sky, at least in German-speaking countries’. Nevertheless, Gertler revealed that, as of September 2014, 3M planned to market the product in Germany and a bit later in the year in Spain.
This will not be the only CAC solution on the German-speaking market, as the Berlin-based company ID GmbH & Co. KGaA is also developing solutions in automated coding. It is good news for the market to have multiple players competing in a region because this will help to further increase awareness of CAC systems, plus bring some downward movement in pricing.
Will coders become jobless?
Stein answers this question with a resolute ‘No, the role of a coder will not become obsolete!’ Although CACs perform most of the task associated with coding, especially on routine procedures, coders address more complex scenarios and audit the suggested codes from a CAC system. ’If anything,’ he concludes, ‘coders’ roles will become more demanding.’
11.11.2014





