Video • Digital twin
Collaboration of the future: and AI makes three
In view of the advent of personalised medicine and holistic therapy many experts predict the end of healthcare as we know it. However, in many places it is ‘healthcare business as usual’. In our interview, Dr Christoph Zindel, President Diagnostic Imaging at Siemens Healthineers, explains where he sees radiology bridging the gap between symptom-centred treatment today and the systemic medicine of tomorrow.

Current therapy approaches are not as local as often made out to be: ‘Indeed there are more systemic illnesses than we think. A weak heart, for example, affects the vascular status and even a malignant tumour cannot be considered a local event. Nevertheless, there are many strong arguments in favour of increasing specialisation, which we also see in radiology. One example: Skeletal scintigraphy in nuclear medicine, a field I have been studying intensively. It evaluates the body as a whole and is thus able to track metastases of breast and prostate cancer via the standard uptake value – SUV.’
Old procedures, new ideas
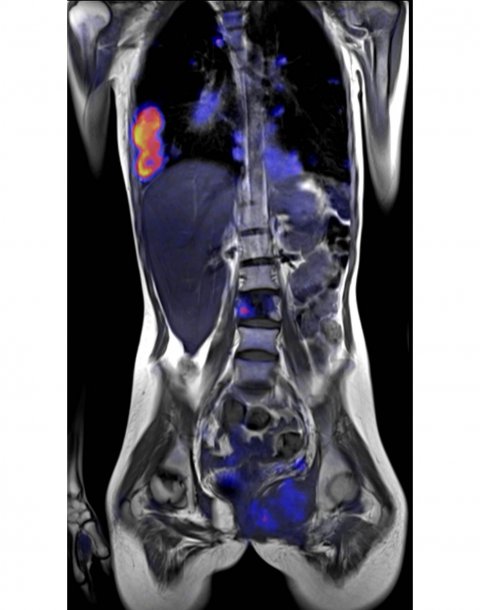
Today, even organ-based modalities such as MRI can be used in a way to offer insights into the entire body, for example when the effects of rheumatoid diseases or diabetes mellitus need to be assessed. ‘Some procedures have been completely rethought,’ Zindel says, and points out that PET/MR, the combination of positron emission tomography and MRI, plays an important role in visualising tumour metabolism.
Whether the holistic perspective or the still widespread practice of treating the symptoms is the road to success depends to a large extent on the type of disease. Zindel is optimistic that new methods, such as gene sequencing and molecular analysis, will offer innovative approaches: ‘Precision medicine will come because we will have ever better tools that can show ever more details and interdependencies.’
Achieving the big picture
To keep track of all the different aspects of personalised diagnostics and treatments, the interaction of different tools is increasingly important, Zindel points out. Case in point: radiomics. ‘Today algorithms can, to a large extent, independently recognise relevant features in image data – the so-called feature extraction. It’s a valuable tool in brain volumetry, for example, since the ventricle surfaces no longer need to be added up manually. The computers do the drudgery. At the same time the different brain regions are labelled automatically, which is very helpful in the diagnosis of neurodegenerative diseases.’ When these and other results, let’s say of liquid biopsy, are linked – or, to be precise, if a computer is asked to link them – a full picture of the patient is generated. This is an immense added value for therapy but also for prevention purposes.
No doubt there are obstacles to overcome, for example non-standardised procedures, such as MRI, where every radiologist uses the sequences and protocols he or she considers most appropriate in any given case. Since there are no reference values, such as Hounsfield units in CT, data integration poses a challenge. ‘Consensus is virtually impossible to reach, since an image that is considered good by a radiologist in the USA, might be viewed sceptically in Asia and Europe,’ Zindel says, but he adds a way out ‘might be MR fingerprinting, which, for the first time, offers quantifiable data.’
A new and crucial role
Not only the cooperation between radiology and pathology will profit from increased standardisation, the patients will also benefit because AI-processed data will provide information the patient can understand
Christoph Zindel
While Zindel, unlike many others in the industry, does not consider artificial intelligence (AI) to be a panacea, he is convinced that it will drive progress in several areas of healthcare: ‘Smartly used, AI has enormous potential, above all when it comes to simplifying and accelerating processes – which in turn will improve productivity.’ While the machine takes on the role of supporter, humans will continue to make the final decisions – a scenario which will not change any time soon, says Zindel. The algorithm for image data analysis can already discard irrelevant images; thus the radiologist has to deal with a much smaller number of images than before. Drudge work, such as the manual counting of lesions, is history since AI performs this task faster and better.
In differential diagnostics, in particular, Zindel expects AT, combined with Big Data and radiogenomics, will trigger quality leaps: ‘Going forward we may well have a troika of physician, patient and AI that jointly stratifies the patient. Not only the cooperation between radiology and pathology will profit from increased standardisation, the patients will also benefit because AI-processed data will provide information the patient can understand.’
In this scenario, Zindel says, the radiologist will assume a new, but still crucial role as a guide navigating the sea of patient data. ‘The important issue about Big Data is not the fact that we need more data, but that we must be able to cull the relevant information from the sheer mass of data.’
In the long run, this development will render proprietary data silos obsolete, since going it alone is not an option with huge data volumes. ‘The future belongs to collaboration; it is the driver that enhances patient welfare.’ Thus, collaboration will be the starting point of future-proof business models – models that are no longer based on services rendered but on value generated.
Profile:
Working with Siemens for over 20 years, Dr Christoph Zindel was appointed President of Diagnostic Imaging at Siemens Healthineers in 2018. As resident in internal medicine, surgery and nuclear medicine he gained invaluable practical experience that helps him in his task of expanding the boundaries of medical imaging with the help of new technologies.
28.06.2019





