Article • Infection - defect - regeneration
Challenges in septic bone surgery
Infections associated with osteosynthesis and prostheses are not to be underestimated: the infection rate is reported to be one to three percent after joint prosthetic surgery and five to 10 percent after osteosyntheses.
Report: Beate Wagner
‘When you include later infections, the rate is twice as high,’ says Professor Andrej Trampuz, infectologist and Head of the Centre for Septic Surgery at the Centre of Musculoskeletal Surgery (CMSC) in Charité, Berlin, Germany. Since the avascular tissue of the implants impairs phagocytes, he points out, ‘A mere 200 bacteria are sufficient to form a resistant biofilm.’
We are currently witnessing a renaissance of local antibiotics therapy
Andrej Trampuz
Biofilms that are a maximum of four to six weeks old are usually caused by highly virulent microbes, such as Staphylococcus aureus, Streptococci or Gram-negative rods that can be easily eradicated without replacement of the implant. By contrast, mature biofilms form low-virulent microbes, such as Staphylococcus epidermidis and Cutibacterium acnes. ‘The older the biofilm, the more difficult pathogen eradication becomes and the more urgent is an implant replacement,’ Trampuz explains.
Sequestrectomy and removal of infected bone material require aggressive debridement, local soft tissue and bone conditioning, one and two-stage exchange as well as post-surgery antibiosis. Efficiency of the antibiotic therapy is closely related to effective debridement and the reduction of pathogen load during surgery. The antibiotics should be bactericidal and biofilm-active and offer good bone penetration and oral bioavailability, such as rifampicin, ciprofloxacin, penicillin, amoxicillin, fosfomycin and gentamicin. ‘We are currently witnessing a renaissance of local antibiotics therapy,’ Trampuz says. ‘Gentamicin and vancomycin can be applied locally in bone cement in a much higher concentration.’ Prophylaxis requires 0.5 to 1.0 g antibiotic per 40 g cement. In the spacer, a dose of 2.0 to 4.0 g per 40 g cement is used.
Professor Ingo Marzi of the Clinic for Trauma Surgery, Hand Surgery and Restorative Surgery at the University of Frankfurt, Germany, adds: ‘Soft tissue coverage is of crucial importance in the therapy of osteosynthesis infections. Secondary reconstruction is most successful in a clean and properly vascularised bone and soft tissue bed.’ Reconstruction entails thorough removal of infected bone material and insufficiently perfused soft tissue, stabilisation of the limb with spacers, surgical closure of the defect with grafts or flap surgery and bone build-up of the impaired bone.

Marzi recommends the Masquelet technique for bone defect management. In this, following thorough bone debridement and soft tissue coverage an antibiotic-loaded bone cement spacer is inserted into the bone defect. In a second intervention, the cement spacer is removed, without damaging the membrane, and the bone defect is filled with a mixture of BMP-7, tricalcium phosphate and endogenous bone. Bone tissue is harvested either from the iliac crest or via RIA technique (Reamer-Irrigator-Aspirator). ‘Compared with other bone reconstruction methods the Masquelet technique is rather quick, even with large diaphyseal and metaphyseal femur or tibia defects,’ Marzi says. Unlike Masquelet himself, who did not apply antibiotics in order to avoid infection masking, Professor Gerhard Schmidmaier of the German University of Heidelberg uses the procedure to deliver bone cement and high doses of gentamicin and vancomycin.
One advantage is improved perfusion: ‘It’s amazing that today we can improve bone perfusion with the help of the Masquelet technique,’ says the interim director of Heidelberg’s Clinic of Orthopaedics and Trauma Surgery. Today, due to periosteum induction bone defects of 20-25 cm heal well. ‘In addition, locally applied high doses of antibiotics ensure that all bacteria are eradicated,’ Schmidmaier points out. ‘Masquelet used his technique solely for membrane induction and enhancement of perfusion, not to treat infections.’
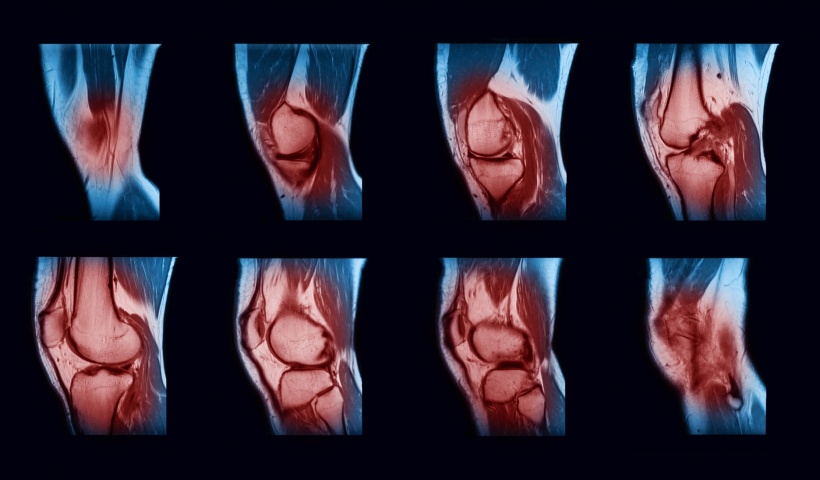
Prior to the intervention cement is prepared in a bowl. ‘This makes the cement a bit more porous and the antibiotic is released better,’ Schmidmaier explains. Nonetheless, he also routinely works with ready-to-use products such as Copa G+V, for example in infected pseudarthrosis. ‘Bone cement loaded with a mixture of gentamicin and vancomycin,’ he explains, ‘catches up to 80 percent of all microbes.’ He recommends that, when placing the bone cement, it makes sense to create irregularly shaped edges on the bone, ‘for the subsequent integration of the new bone, the bone cement should overlap onto the healthy bone material’. When the bone cement is removed after six to eight weeks, the objective is to spare the membrane.
For harvesting graft material Schmidmaier favours RIA, a procedure that allows acquisition of large volumes (20-75 ml) of high-quality autologous bone tissue. ‘Research indicates,’ he points out that morbidity decreases with harvesting using the RIA technique.’ In conclusion, he says: ‘The Masquelet technique is suited for interventions with plates and nails but also in recent trauma. It makes sense from a biological point of view and the combination of gentamicin and vancomycin offers benefits. If a tissue sample is loaded with bacteria that do not respond to the antibiotics, the spacer can be replaced or a suitable antibiotic can be applied locally.’
15.12.2017