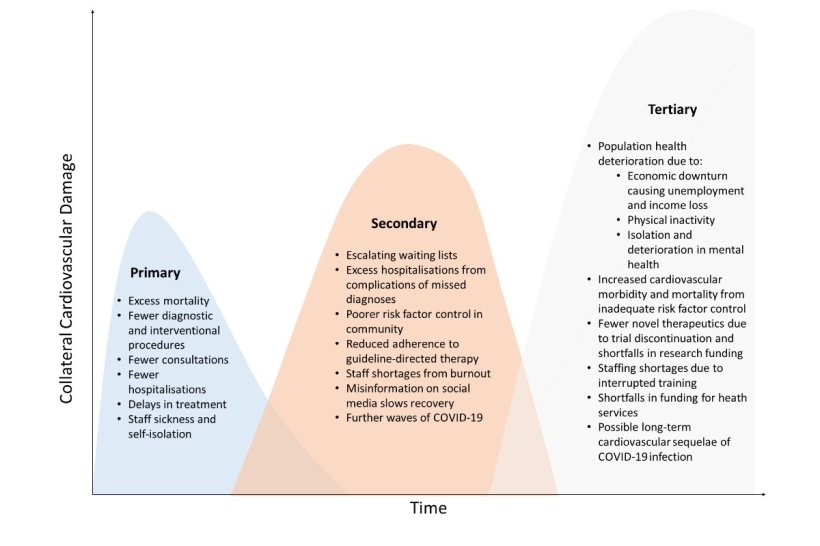
Source: "Graphic courtesy of the European Heart Journal"
News • Cardiac care
Cardiac disease expected to worsen post corona pandemic
A major international study has revealed the “global collateral damage” caused by the disruption to cardiac services from the COVID-19 pandemic. The researchers, led by the University of Leeds, warn that across the world problems with heart health will “...continue to accrue unless mitigation strategies are speedily implemented”.
The British Heart Foundation says the study is evidence of further pressure on already overwhelmed cardiac services in England, with more than 300,000 people now waiting for treatment.
In the two years from December 2019, when health systems around the world were under extreme pressure and people were fearful of catching COVID-19, individuals experiencing an acute cardiac event such as a heart attack or heart failure either stayed away or could not get admitted to a hospital.
The study describes a “substantial global decline” in hospital admissions of people suffering from cardiovascular disease. As a result, the number of people dying at home or in the community from heart conditions increased.
In cases where people did get medical help there was, on average, more than an hour’s delay in reaching hospital or having contact with paramedics. The chances of people surviving a major heart attack depends on timely and appropriate treatment.
Although the problems identified by the researchers were seen across the world, they were exacerbated in low to middle income countries.
Hospitals and clinics in those locations struggled to give the gold standard treatment, in some cases using drugs instead of interventional procedures such as fitting a stent into a blocked artery. The result has been an increased death rate among cardiovascular patients in hospitals in low to middle income countries, as well as more people dying at home from cardiovascular disease in the UK.
Involving an international team of doctors and data scientists led by the University of Leeds, the study gives the first global assessment of the way cardiovascular services coped during the pandemic.
Recommended article

News • Cardiology research
Covid-19 vaccine technique could also save tissue after heart attack
A method for delivering genetic material to the body that has proven useful in Covid-19 vaccination is now being tested as a way to repair damaged heart muscle after a heart attack.
"Urgent plan needed for cardiac services"
The British Heart Foundation says here is a need for an urgent plan to help cardiac services in England deal with the increasing number of people who now need treatment. Figures from the BHF show that at the end of March, 309,796 people were on a waiting list for cardiac treatment in England – a figure that has been growing over the previous 21 months.
Dr Sonya Babu-Narayan, Associate Medical Director at the BHF and consultant cardiologist, said: “We need a comprehensive and specific cardiovascular plan to address the burden of cardiovascular care including the backlog - and provide immediate and long-term solutions to our cardiovascular workforce shortage. Without this we will continue to see heart attacks, lasting heart damage, or even premature deaths that could have been avoided.”
The team analysed data from 189 separate research papers looking at COVID-19's impact on cardiovascular services from 48 countries on six continents and covering a two-year period from December 2019.
“Heart disease is the number one killer in most countries – and the analysis shows that during the pandemic, people across the world did not receive the cardiac care they should have received," Dr Ramesh Nadarajah, a British Heart Foundation Clinical Research Fellow at the University of Leeds and lead author of the paper, said. "That will have ramifications. “The longer people wait for treatment for a heart attack, the greater the damage to their heart muscle, causing complications that can be fatal or cause chronic ill health. Health systems need to be reinforced so they can support and treat people whose heart conditions will inevitably be worse because of the pandemic. The paper provides evidence of that.”
Previous systemic reviews of the impact of COVID-19 on cardiovascular services have presented an “incomplete overview”, say the researchers. To address that, they comprehensively investigated a range of heart services across regions, from hospitalisations, heart disease management, diagnostic procedures, outpatient consultations and mortality rates. They combined data from multiple studies to give a value for the number of cases hospitals and clinics were seeing compared to the expected caseload if there wasn’t a pandemic.
Data from low to middle income countries is sparse and the researchers believe their findings underplay the true extent of the impact of COVID-19 disruption on heart services in low to middle income countries.
Recommended article
News • Revealed via new x-ray technique
Covid-19 can cause vascular damage to the heart
Using a new x-ray imaging approach, an interdisciplinary research team has detected significant changes in the heart muscle tissue of people who died from Covid-19.
Headline findings from the research
Because of the different way the statistics in the survey had been collated, the researchers used percentages to compare services.
Hospitalisations
- Globally, hospitals saw a 22% decline in people experiencing a serious heart attack where one of the arteries serving the heart is completely blocked (STEMI heart attack).
- There was 34% decline in people attending hospital with a less severe form of heart attack, where an artery is partially blocked (NSTEMI heart attack).
- The drop in patients was not due to fewer heart attacks but fewer people attending hospital for treatment.
- The decline in people attending hospital was seen around the world but was greater in low to middle income countries.
Treatment delays
- On average, it was taking patients 69 minutes longer to receive medical assistance for a serious heart attack after the start of their symptoms.
Management of a heart attack
- The gold standard treatment for many heart attack patients is to have a stent inserted into the blocked artery. In many low to middle income countries there was a sharp decline in those procedures being carried out: in just 73% of cases where the patient was having a major heart attack and 69% of cases where the patient was suffering a less severe heart attack. There was a shift to treat patients with clot busting drugs instead.
Heart operations
- Globally, there was a 34% drop in heart operations.
Interventional procedures
- Just over half (51%) of the electronic implantable devices, such as pacemakers, used to control abnormal heart rhythms were fitted when compared to the non-COVID-19 period.
Deaths due to heart disease
- Globally, among patients in hospital after having had a major heart attack or heart failure, the number of people dying from any cause was up by 17%. This was driven by an increase in the death rates among cardiovascular patients in low to middle income countries.
- Studies from the early phase of the pandemic in the UK revealed a “displacement of death” effect where more people were dying from acute coronary events at home – running at 31% rather than the expected 24%. In care homes, the figures were 16% versus 14%.
The study is published in the European Heart Journal.
Source: University of Leeds
31.05.2022