Breast Specific Gamma Imaging Supports Mammography
By Kerry Heacox, i.t. Communications
Breast-specific gamma imaging (BSGI) is a promising new technology designed to supplement mammography and breast ultrasound examinations when these show suspicious findings. By helping to detect early stage breast cancer it may reduce significantly the number of negative biopsies performed. Dilon Technologies (Newport News, Virginia), pioneer of this technology, received the CE Mark to sell its camera in the EU in June 2008, and it is already in use in Belgium, France, Sweden and Turkey.
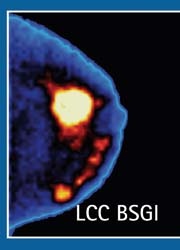
BSGI images the metabolic activity of breast lesions through radiotracer (99m-technetium sestamibi) uptake. It uses a high resolution gamma camera to detect subcentimetre breast cancers even less than 5 mm. Breast cancer is identified based on the differential uptake of radiotracer in cancer cells as compared with normal surrounding breast tissue.
This procedure provides an easy, rapid and economic way to perform supplemental breast imaging of women with dense breast tissue, cosmetic implants, post-surgical scars and masses, multiple suspicious lesions, and palpable lesions not detected by mammography and ultrasound. Although a breast may be imaged in any position during a BSGI exam, it is designed to replicate positions used in mammography, specifically craniocaudal and mediolateral oblique projections. Unlike an MRI procedure, which may acquire hundreds of images, a typical BSGI exam only has 4-16 images, and can be reviewed and interpreted more rapidly by a radiologist. A typical BSGI procedure takes about 40 minutes.
The American Cancer Society recommends that women at high risk for breast cancer have an annual MRI exam. Since BSGI represents a more reliable procedure, is far less expensive to buy and exams cost about a third less than MRI’s, it increasingly utilised in lieu of MRI exams for some patients by US hospitals and women’s imaging centres.
BSGI also may be more suitably used for patients who are claustrophobic, very obese, have pacemakers or other ferromagnetic implants, and who have renal conditions, which may be adversely affected by contrast agents used for MRI exams. Same-day scheduling is also possible at many facilities, ending a long wait for heavily utilized MRI equipment.
Professor of Radiology Dr Rachel F Brem, Director of Breast Imaging and Intervention at George Washington University Medical Center in Washington D.C., has led the academic research evaluations of BSGI technology. In the first peer-review published study (Radiology, Vol. 247, No. 3, June 2008) evaluating 83 pathologically confirmed malignant lesions out of 167 total biopsied lesions with no mammographic correlation, BSGI images helped radiologists to identify 80 as malignant, resulting in a sensitivity of 96.4%. In the 84 non-malignant lesions, it identified 50 as negative, with a specificity of 59.5%. The BSGI procedures helped detect occult cancers in six patients that were not identified with either mammography or ultrasound.
At RSNA 2008, Prof Brem presented results of a study to determine how often BSGI identifies additional unsuspected areas of breast cancer in women with one confirmed breast tumour. 159 women between the ages of 29 to 93, 73% of whom had dense breasts, were imaged with BSGI. It identified 56 additional occult suspicious lesions. When biopsied, nine previously unidentified cancers were found in the same breast and five cancers in the opposite breast. BSGI identified an additional 9% of occult cancers that would otherwise not have been detected.
BSGI is showing potential identifying invasive lobular carcinoma. A study (pub: 2/09 issue of AJR. Vol. 192) compared the results of sonography, MRI and BSGI in identifying 28 invasive lobular carcinomas found in 26 patients who had breast exams at two academic hospitals and two imaging centres. BSGI had a sensitivity of 93%; MRI 83%; mammography 79% and sonography 68%.
BSGI is being used in surgical planning. The increased trend to perform less invasive breast conservation surgery and more focused radiotherapy, when required, necessitates defining the extent of breast disease very precisely. MRI offers high sensitivity to detect additional lesions and provides morphologic detail of anatomy and its extent of disease, but its high level of false positives often requires additional imaging.
In a 12-month study of 138 newly diagnosed patients with early stage breast cancer, two community breast imaging centres of Legacy Health System in Portland, Oregon, had BSGI exams as well as MRI exams. MRI sensitivity was 83%, whereas BSGI sensitivity was 93%, detecting 26 of the 28 lesions. BSGI also identified additional cancers in 25 of the patients. Eight cancers were in the ipsilateral breast and seven cancers were identified in the contralateral breast. Clinical surgical management was changed as a result for eight patients, including a conversion from breast conservation to mastectomy. The study results were published in the American Journal of Surgery (Vol. 197, February 2009).
01.07.2009





