Article • Hypertension and CVD assessment and prediction
Blood pressure measurement: deceivingly simple, yet highly complex
Blood pressure (BP) is one of the most basic parameters in any healthcare status assessment and holds considerable diagnostic significance. However, clinicians should never underestimate the complexity behind the assessment, cautions Dr Rhian M. Touyz, MBBCh, PhD. At the ESC congress in Barcelona, the expert from the Research Institute of the McGill University Health Centre (RI-MUHC) in Montréal, Canada, went into detail on the implications of time and variability in BP measurement, challenging the conception of longer measurements always yielding superior results.
Report: Wolfgang Behrends

© McGill University Health Centre
A major challenge in blood pressure measurement is achieving accurate and reproducible results, while finding practical solutions for the clinical setting at the same time. ‘One can’t emphasize enough the importance of accurate blood pressure measurement,’ she stressed. Not only is it essential to reliably diagnose hypertension, but also to predict and manage cardiovascular risk. The value affects when and how a patient is treated, and it reflects on how well a patient responds to therapy.
However, blood pressure is far from static, but is influenced by a patient’s physiology, circadian rhythm and posture, measurement environment and method, as well as many additional factors. For example, a patient who has just had a meal will present with a slightly lowered systolic BP reading due to ingestion, while caffeine intake, exposure to cold or the mere presence of an observer is known to raise blood pressure.1 It is vital to take this huge variability into account, Touyz pointed out.
Measurement inaccuracy: more than just a cosmetic error
The current gold standard to assess a patient’s BP is through intra-arterial measurement – an impractical method due to its highly invasive nature. Therefore, practically all clinical institutions rely on indirect alternatives, and office BP measurements are mostly performed using automatic oscillometric devices with a brachial cuff.
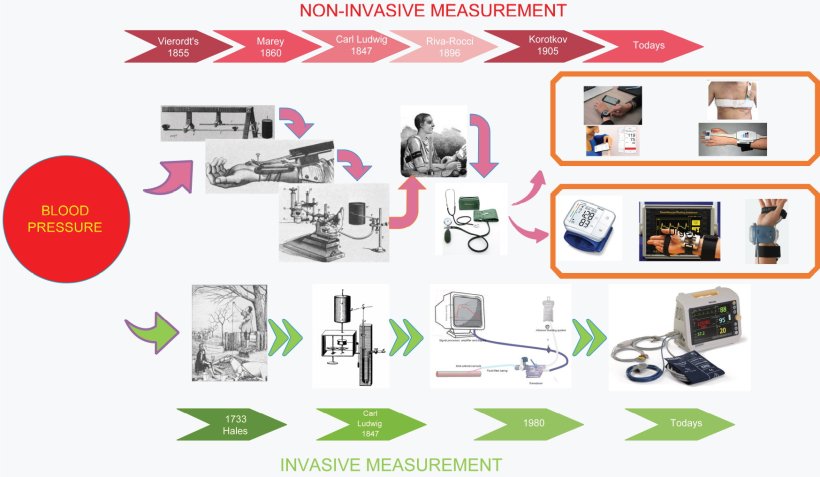
Image source: Şentürk et al., Turkish Journal of Electrical Engineering and Computer Sciences 2019 (CC BY 4.0)
While this is in accordance with the International Society for Hypertension’s best practice guidelines2, medical professionals should be aware of the limitations, Touyz cautioned: ‘This is a snapshot measurement, so there is a failure to capture the variability in blood pressure.’ Another factor to keep in mind is white coat hypertension, which has 15-25% of patients present with higher BP simply because the reading is performed in an unfamiliar setting, such as the GP’s office. On the opposite side, these measurements may underdiagnose so-called “masked hypertension”, where blood pressure is uncharacteristically low during the patient’s office visit.
The expert made it clear that these fluctuations are not to be dismissed easily: ‘Inaccuracies of just 5 mmHg correspond to an incorrect classification of hypertension in 84 million people worldwide.3 The economic, societal and individual impact is huge, so we do have to measure blood pressure accurately and we do need to consider all these variables.’
Home-based measurement: device validation is essential
A possible way out of the problem comes in the form of automated and out-of-office blood pressure measurement, Touyz suggested. According to current recommendations, most automated devices measure BP several times with 1-minute intervals. Recent research even suggests that repeated measurements achieve comparable accuracy with only 30-second intervals.4 On the other hand, studies with extended intervals beyond one minute did not observe improved results.5

Image source: Adobe Stock/Microgen
Various types of devices for home-based BP measurement have seen widespread use, not least due to the Covid-19 pandemic. Not only is this method practical and convenient, but also predictive of cardiovascular events, the experts said. ‘It is actually a very good method for long term follow up of treated patients.’ She also welcomed that self-measuring contributes to a sense of involvement and ownership in a patient’s care. ‘But it is absolutely essential that these home blood pressure devices are accurately validated.’ The expert emphasized this aspect in view of a recent Australian study that found the majority of commercially available devices to not be proven accurate according to international validation standards.6 She therefore appealed to her colleagues to only recommend devices to their patients that have been validated by institutions such as the British and Irish Hypertension Society7 or the German Hochdruckliga8.
Upcoming technologies
In the coming years, the field might benefit from the introduction of promising new technologies, Touyz predicted. Case in point: researchers currently explore the potential of graphene tattoos, which noninvasively measure the bioimpedance between the radial and ulnar arteries and use an algorithm to assess blood pressure.9 This system, which can measure BP continuously for more than 300 minutes, shows how new technology could address current challenges in terms of BP variability, the expert concluded.
‘The most important message is to be aware of the impact of variability,’ she pointed out, urging clinicians not to think of blood pressure as just one number that defines the risk of hypertension. Sharing this knowledge with patients is another critical factor, as patients tend to get confused when their BP values are different across several measurements. ‘It is important to make patients aware that variability is normal, but that blood pressure should be measured at the same time of day and under the same conditions.’
References:
- Kallioinen et al.: Sources of inaccuracy in the measurement of adult patients’ resting blood pressure in clinical settings: a systematic review; Journal of Hypertension 2017
- Unger et al.: 2020 International Society of Hypertension Global Hypertension Practice Guidelines; Hypertension 2020
- Padwal et al.: Optimizing observer performance of clinic blood pressure measurement: a position statement from the Lancet Commission on Hypertension Group; Journal of Hypertension 2019
- Juraschek et al.: Impact of 30- Versus 60-Second Time Intervals Between Automated Office Blood Pressure Measurements on Measured Blood Pressure: Hypertension 2021
- Imamura et al.: Effects of measurement intervals on the values of repeated auscultatory blood pressure measurements: Clinical and Experimental Hypertension 2020
- Picone et al.: Nonvalidated Home Blood Pressure Devices Dominate the Online Marketplace in Australia: Major Implications for Cardiovascular Risk Management: Hypertension 2020
- British and Irish Hypertension Society – list of validated BP monitors
- Deutsche Hochdruckliga – Blutdruckmessgeräte mit geprüfter Sicherheit
- Kireev et al.: Continuous cuffless monitoring of arterial blood pressure via graphene bioimpedance tattoos; Nature Nanotechnology 2022
06.10.2022