Antibiotic resistance spreads rapidly between bacteria
The part of bacterial DNA that often carries antibiotic resistance is a master at moving between different types of bacteria and adapting to widely differing bacterial species, shows a study made by a research team at the University of Gothenburg in cooperation with Chalmers University of Technology. The results are published in an article in the scientific journal Nature Communications.
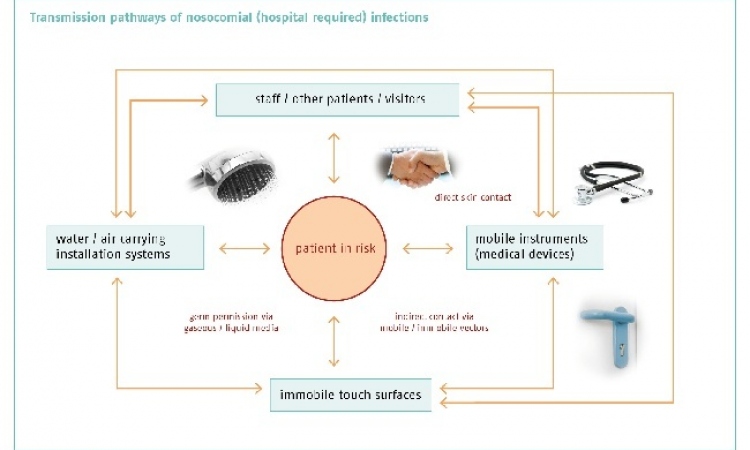
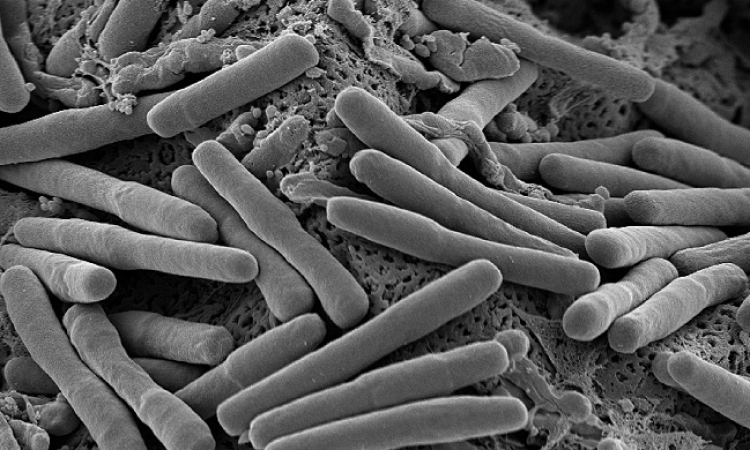
More and more bacteria are becoming resistant to our common antibiotics, and to make matters worse, more and more are becoming resistant to all known antibiotics. The problem is known as multi-resistance, and is generally described as one of the most significant future threats to public health Antibiotic resistance can arise in bacteria in our environment and in our bodies. Antibiotic resistance can then be transferred to the bacteria that cause human diseases, even if the bacteria are not related to each other.
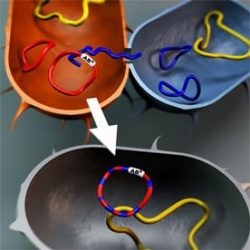
A large proportion of gene transfer between bacteria takes place with the aid of what are known as conjugative plasmids, a part of the bacterial DNA. A plasmid can only exist and multiply inside a cell, where it uses the cell’s machinery, but can then be transferred to another cell and in that way spread between bacteria.
The research team has studied a group of the known carriers of antibiotic resistance genes: IncP-1 plasmids. Using advanced DNA analysis, the researchers have succeeded in mapping the origin of different IncP-1 plasmids and their mobility between different bacterial species. “Our results show that plasmids from the IncP-1 group have existed in, and adapted to, widely differing bacteria. They have also recombined, which means that a single plasmid can be regarded as a composite jigsaw puzzle of genes, each of which has adapted to different bacterial species”, says Peter Norberg, a researcher in the Institute of Biomedicine at the University of Gothenburg. This indicates very good adaptability and suggests that these plasmids can move relatively freely between, and thrive in, widely differing bacterial species.
“IncP-1 plasmids are very potent ‘vehicles’ for transporting antibiotic resistance genes between bacterial species. Therefore, it does not matter much in what environment, in what part of the world, or in what bacterial species antibiotic resistance arises. Resistance genes could relatively easily be transported from the original environment to bacteria that infect humans, through IncP-1 plasmids, or other plasmids with similar properties, as ‘vehicles’,” says Professor Malte Hermansson of the Department of Cell and Molecular Biology at the University of Gothenburg.
It has been known for some time that plasmids are important in the spread of antibiotic resistance. The research team’s findings show that IncP-1 plasmids can move, and have moved, between widely differing bacterial species and in addition have interacted directly with one another, which can increase the potential for gene spreading.
The study "The IncP-1 Plasmid Backbone Adapts to Different Host Bacterial Species and Evolves Through Homologous Recombination" has been conducted by Peter Norberg, Maria Bergström and Malte Hermansson at the University of Gothenburg, in cooperation with Vinay Jethava and Devdatt Dubhashi at the Chalmers University of Technology.
18.04.2011