Article • Cardiology
AI system improves heart disease diagnosis
Cardiologists in the UK are trialling an artificial intelligence (AI) system that will help better diagnose heart disease.
Report: Mark Nicholls

Devised by researchers from the University of Oxford, it can predict heart disease and cardiac events from ultrasound stress test images with initial results showing that the AI system is far more accurate than conventional techniques.
Paul Leeson, Professor of Cardiovascular Medicine at the University of Oxford - who leads the development team with PhD student Ross Upton - said the system is currently being trialled in a “real world cardiology” environment in 15 units across the UK to formally assess its effectiveness and accuracy ahead of a formal publication of the results and a clinical roll-out.
With current examination techniques, it is estimated that the diagnosis is wrong in up to 20% of cases, leading to patients either being sent home with the risk of having a cardiac event, or undergoing unnecessary procedures.
With knowledge of background history and what happens to them subsequently, you can start to pick out very interesting predictors of who gets disease and who does not
Paul Leeson
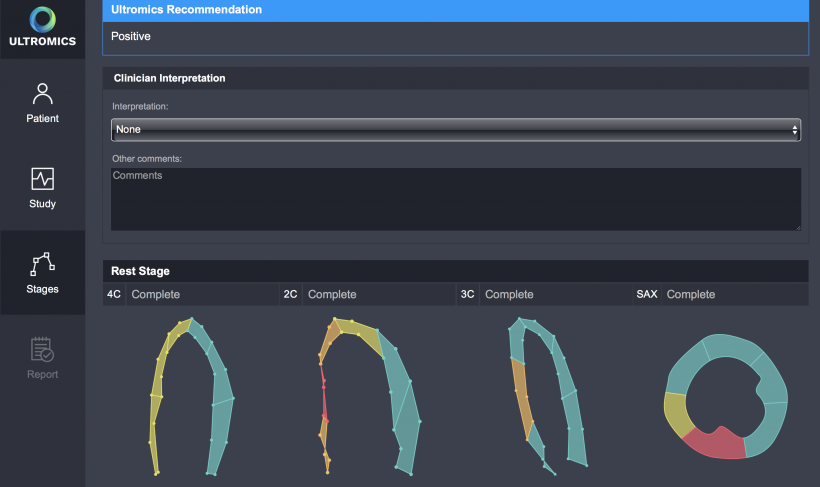
The new AI system, developed from ongoing research studies at the University of Oxford Cardiovascular Research Facility, is set to significantly improve upon that. The company developing the technology is called Ultromics and the stress echo analysis software is called Echuity and is ultrasound vendor neutral in that it works with images from any of the major ultrasound manufacturers. The process to construct the diagnostic algorithm involved extracting thousands of parameters from echocardiogram images and using machine learning to determine which parameters were most diagnostic of coronary artery disease. From that, the system gives a diagnostic recommendation to the clinician on whether it believes there is the risk of a patient having a heart attack or not, and identifies the location of disease.
Professor Leeson, who is also a Consultant Cardiologist at the John Radcliffe Hospital and Professor of Cardiovascular Medicine at the University of Oxford, said: “Ultrasound and stress echo are one of the most widely used imaging modalities to investigate heart disease. At the moment as cardiologists, we look at these images and try and identify changes with the eye. We are pretty good at doing that but my feeling was that we could do this better.”
By revisiting images and working with returning patients, they have been able to extract additional information to look at different biomarkers and approaches to try to improve stress echo findings. He continued: “With a particular focus on ultrasound image data, we have broken that down into different bits to see what parameters we can pull out of these echo images. Because we had follow up extending over many years we were able to take that ultrasound imagery and see what features are predicting who has events and who does not when a patient comes forward for stress echo. With knowledge of background history and what happens to them subsequently, you can start to pick out very interesting predictors of who gets disease and who does not.” What emerged were good imaging biomarkers that could be applied prospectively within an algorithm to identify individuals who are most likely to suffer heart disease or have a cardiac event.
From images of the heart, the team developed ways of applying these techniques to provide accurate and a consistent results. To date, the system has an accuracy level equivalent to the best performing clinicians of a one in 10 error rate, but the researchers are keen to rigorously test this. That involved comparing how accurately clinicians are predicting outcome with how accurately the machine algorithm approach predicts outcome in 15 cardiology departments. However, Professor Leeson stressed: “We know we can get good results based on the data we have from our centre. What we want to do at this stage is confirm that the automated approach consistently produces at least as good results as the best quality operator. Of course, the cardiologist will still need to decide what to tell the patient and work out what the best management plan for the patient may be, but for the patient, increased accuracy may save unnecessary invasive procedures such as angiograms. It will also see less patients being sent home with coronary artery disease when they should have been sent for angiograms.”
With about 60,000 heart scans carried out annually, with 12,000 misdiagnosed, the cost to the NHS is £600m in unnecessary operations and the treatment of people who had heart attacks following an all-clear scan. With AI making more accurate diagnoses, the team believes that could save the NHS more than £300m a year with the reduction in misdiagnosis.
Profile:
Paul Leeson is Professor of Cardiovascular Medicine at the University of Oxford and a Consultant Cardiologist at the John Radcliffe Hospital. He heads the Preventive Cardiology Research Group at the Oxford Cardiovascular Clinical Research Facility, which aims to improve identification and prevention of heart disease in young people via: novel markers of early disease, young adult cardiovascular prevention trials, and artificial intelligence.
11.11.2018





