News • Machine learning vs. NSCLC
AI to improve post-treatment surveillance of lung cancer patients
Artificial intelligence (AI) could help guide the post-treatment surveillance of non-small cell lung cancer (NSCLC) patients and improve outcomes as a result, according to a study led by researchers from The Royal Marsden NHS Foundation Trust in collaboration with The Institute of Cancer Research, London, and Imperial College London.
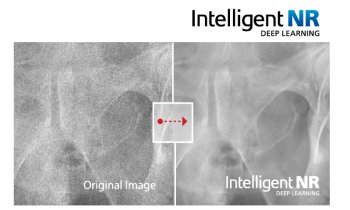
In a world-first, the OCTAPUS-AI study, published in the Lancet’s EbioMedicine journal, compared different machine learning models to determine which could most accurately identify NSCLC patients at risk of recurrence following curative radiotherapy. Machine learning (ML) is a type of AI that allows software to automatically predict outcomes. ML algorithms build a model based on sample data to make predictions or decisions without being explicitly programmed to do so.
Results from the retrospective, multicentre study suggest that this technology could be used to help personalise and therefore improve the surveillance of patients following treatment based on their risk. This could lead to recurrence being detected earlier in high-risk patients, ensuring that they receive urgent treatment which could potentially improve their outcomes. For those with a low risk of recurrence, it could result in fewer follow-up scans and hospital visits.
This study shows that machine learning models can predict NSCLC patients’ outcomes following curative radiotherapy using routinely available clinical data
Sumeet Hindocha
The researchers used anonymised, routinely available clinical data from 657 NSCLC patients treated at five UK hospitals to compare different machine learning algorithms based on various prognostic factors – used to predict a patient’s chance of recurrence - such as age, gender, and the tumour’s characteristics on scans. They then developed and tested prediction models to categorise patients into low and high risk of recurrence, recurrence-free survival, and overall survival at two years post treatment. For example, researchers found that the patient’s tumour size and stage, type, and intensity of radiotherapy, smoking status, BMI and age were the most important factors in the final model’s algorithm for predicting patient outcomes. This model was also found to be more accurate in predicting outcomes than traditional methods such as the TNM staging system, which describes the amount and spread of cancer in a patient's body.
Lung cancer is the leading worldwide cause of cancer death and accounts for just over a fifth (21 per cent) of cancer deaths in the UK. NSCLC makes up nearly five sixths (85 per cent) of lung cancer cases and, when caught early, the disease is often curable. However, over a third (36 per cent) of NSCLC patients experience recurrence in the UK.
To improve the outcomes of lung cancer patients, the National Institute of Healthcare and Clinical Excellence (NICE) has called for further research into using prognostic factors to develop risk-stratification models to inform optimal surveillance. The OCTAPUS-AI study was developed in response to this recommendation. Study lead Dr Sumeet Hindocha, Clinical Oncology Specialist Registrar at The Royal Marsden NHS Foundation Trust and Imperial College London, said: “Right now, there is no set framework for the surveillance of non-small cell lung cancer patients following radiotherapy treatment in the UK. This means there is variation in the type and frequency of follow-up that patients receive. More research is required to develop personalised follow-up protocols and using AI with healthcare data may be the answer.
“This study shows that machine learning models can predict NSCLC patients’ outcomes following curative radiotherapy using routinely available clinical data. As this type of data can be accessed easily, this methodology could be replicated across different health systems. This study is therefore an exciting first step towards developing a model to help guide the post-treatment surveillance of this patient group based on their individual risk of recurrence. The next phase of this study will test machine learning models using imaging data alone and in combination with clinical data. We hope to find out how our model, which is based on patient characteristics and the treatment they received, is influenced by imaging scan data”.
Dr Richard Lee, Consultant Physician in Respiratory Medicine and Early Diagnosis at The Royal Marsden NHS Foundation Trust and Team Leader for the Early Diagnosis and Detection team at The Institute of Cancer Research, London, who is chief investigator for the OCTAPUS-AI study, said: “This is an important step forward in being able to use AI to understand which patients are at highest risk of cancer recurrence, and to detect this relapse sooner so that re-treatment can be more effective. Relapse is also a key source of anxiety for patients. Reducing the number of scans needed in this setting can be helpful, and also reduce radiation exposure, hospital visits, and make more efficient use of valuable NHS resources. In the future, we hope this approach will pave the way for predicting recurrence for all cancer types, not just NSCLC. Our model used features specific to this disease but by refining the algorithm, this technology could have much wider application. Through this work, we hope to push boundaries to improve the care of cancer patients, to help them live longer, and reduce the impact the disease has on their lives. We are grateful to our patients and donors who have made this research possible.”
This study was supported by the Early Diagnosis and Detection Centre which aims to accelerate early diagnosis of cancer. The Centre has been established in partnership with the ICR, hosted by the National Institute for Health Research Biomedical Research Centre (NIHR BRC) and is supported by funding from The Royal Marsden Cancer Charity. The Early Diagnosis and Detection Centre brings together early detection research and expertise across multiple tumour groups.It focuses on identifying higher risk groups, who will then benefit from AI, imaging, and novel liquid biopsy technologies, helping to detect cancers earlier, faster and to give a more accurate diagnosis.
Source: Institute of Cancer Research
26.04.2022