Article • From observation to action
The rise of agentic AI in pathology
Computational pathology is becoming increasingly important in helping deliver precision medicine to a wider range of patients. Experts at the 37th European Congress of Pathology in Vienna discussed how algorithms can optimise laboratory workflows, generate stronger evidence for molecular tumour boards, and enhance clinical trial design.
By Mark Nicholls
© tadamichi – stock.adobe.com

Photo courtesy of Prof Brevet
Pathologist Marie Brevet emphasised how computational algorithms can optimise workflow and generate clinical impact by integrating data across the entire pipeline rather than focusing on a single model. She also discussed near-future perspectives involving foundation models, multimodal approaches, and the emerging role of agentic AI.
Brevet, who is founder and CEO of health innovation company Biwako, said use of Natural Language Processing (NLP) in pathology can digitise request forms and generate medical reports with AI as a virtual secretary for pathologists.
Saving time, reducing errors
Acknowledging that challenges remain in how to integrate such models into Laboratory Management Systems (LMS), she said that large language models (LLMs) will save pathologists time and decrease transcription errors. Within the context of workflow, computational algorithms can support case triage, balance workload and enable real-time tracking and monitoring of laboratory processes, detecting mismatches and flagging errors with automated quality control.
'An example in dermatopathology is with the use of algorithms that not only predict the likelihood of melanoma or carcinoma but can also prioritise the most urgent cases,' she said.
Brevet also underlined how, in practice, a laboratory can automatically route melanocytic lesions to its local expert, ensuring faster and more accurate decision-making.
Foundation models and agentic AI
While that may feel both intimidating and fascinating, agentic AI is closer than many imagine
Marie Brevet
In molecular pathology, algorithms can prioritise cases most likely to benefit from targeted therapies and enrich the pool of patients for DNA or RNA sequencing. Meanwhile, foundation models are reshaping the field of pathology. Trained on vast and heterogeneous datasets, they are designed as pre-trained architectures that can be rapidly fine-tuned for multiple downstream tasks. 'The benefit,' explained Brevet, 'is that they do not begin every new task from scratch, which allows scalability and robustness.'
While generative AI creates content, she described how agentic AI can go a step further and 'decide, act, and interact' with other systems – moving from 'observation to action' – such as drafting a medical report autonomously without human request. 'Agentic AI can have a global view of a laboratory, identify where bottlenecks occur, and then observe, decide and execute the necessary actions to avoid them. While that may feel both intimidating and fascinating, agentic AI is closer than many imagine.'
Multimodal data for molecular tumour boards
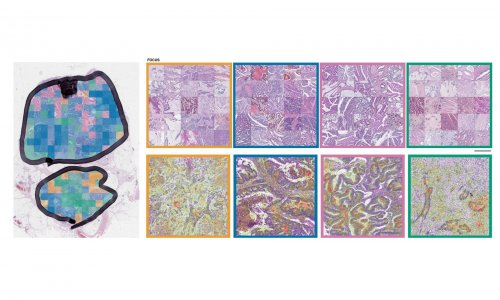
Image source: Institut National Genevois
Professor Olivier Michielin explained how a multimodal approach can deliver better, more specific information to molecular tumour boards (MTBs) and facilitate precision medicine. Michielin, who is Head of the Department of Oncology and the Precision Oncology Service at Geneva University Hospital, discussed an approach to integrate multiple data streams into a precision oncology programme that would see patients split into well-defined populations so they are 'exquisitely sensitive' to a given therapeutic intervention.
In his presentation on 'The integrative/multimodal tumour board for improved precision medicine,' he said: 'This could lead to massive benefits for patients. It is still a bit of a dream…but we are getting there.'
With data science at the core, the challenge is how to standardise data streams from clinical data, patient-reported outcomes, multiomics, spatial omics, digital pathology and radiomics. While it is a long process, it could see information placed before experts on the MTB for precision oncology to decide on the best treatment option for a patient. Building on that, the data would be retained to enrich decision-making processes going forward.
Spatial biomarkers and longitudinal data
A significant step has been the creation of the Swiss Personalised Oncology (SPO) network across major hospitals and universities using structured data or NLP to extract information from medical records in diverse systems. 'We can extract data and follow patients longitudinally, which provides time-bound information that can be analysed with process mining technology and follow, for example, how patients are distributing across treatment lines. We believe the spatial component of multiomics will be key – spatial biomarkers are indeed predictive of benefits of immunotherapy in melanoma, lung, as well as other cancer types sensitive to immunotherapy.'
We are convinced that the best use of these rich data and multidimensional datasets will allow us to raise the bar in therapy
Olivier Michielin
Given the importance of the spatial component, his department has created a spatial workflow applicable on digitalised or physical slides. He showed an example of his fully digitalised approach with the development of a predictive image-based digital pathology biomarker for IO therapy response in metastatic melanoma.
Building tools for interactive tumour boards
A national omics network has been built in Switzerland to recruit 300 patients, with patients' treatment decided based on next-generation sequencing programmes, spatial-omics, digital pathology and drug screening. He illustrated examples of how the approach may help improve treatment and deliver precision medicine therapies for patients.
Michielin added: 'Being able to bring information to the molecular tumour board and discussing it interactively with the doctors and data scientists is essential. We are also building tools that allow us to view and interact with the data at the tumour board. We are convinced that the best use of these rich data and multidimensional datasets will allow us to raise the bar in therapy.'
Digital twins and clinical trials
Professor Albino Eccher from the University of Modena and Reggio Emilia outlined the potential of digital twins for precision medicine – a technology that connects real-world processes with virtual representation. But while digital twins have moved from 'idea to reality much faster in recent years,' he said their potential is still not fully explored.
Johan Hartman, Professor of Tumour Pathology at Karolinska Institute in Stockholm, Sweden, looked at the role of computational pathology in clinical trials, pointing to its value in automated biomarker qualification, tumour microenvironment analysis, prognostic and predictive modelling and quality control.
Profiles:
Professor Marie Brevet is a pathologist and the founder and CEO of Biwako, a company supporting health innovation. She was Professor and Hospital Practitioner at the University Hospital of Lyon until 2020 and now works with Technipath, Synlab. Her expertise spans the molecular biology of tumours, biobanking, digital health and artificial intelligence. She is also a board member of the French Society of Pathology.
Professor Olivier Michielin is Head of the Department of Oncology and Precision Oncology Service at Geneva University Hospital, Co-Director of the Swiss Cancer Centre Léman and Professor at the Swiss Federal Institute of Technology in Lausanne (EPFL). His research focuses on translational oncology and precision medicine.
03.02.2026