A new imaging tool?
Mammography is the common way to detect breast cancer. But it's not perfect: it struggles to image dense glandular tissue or early-stage tumours. Magnetic resonance imaging (MRI) offers best sensivity but it is expensiv and not always specific enough. Now researchers have come up with another option: a scanner that integrates thermoacoustic and photoacoustic tomography to achieve dual-contrast imaging.
The non-ionizing scanner can potentially provide high-resolution, dual-modality breast imaging.
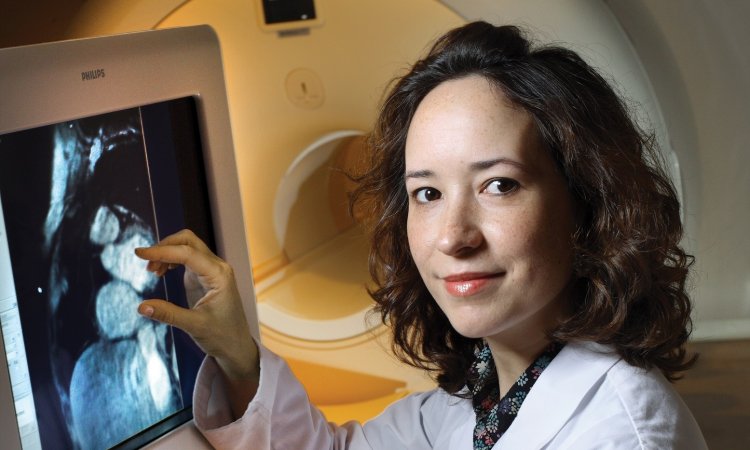
Early diagnosis and treatment are key to surviving breast cancer. Advances in mammography screening and treatment technologies have reduced the death rate of this disease by about 20%. But particulary for high-risk patients the examination by mammography might be sufficient, several studies indcate. Last year, the American Cancer Assiociation issued new guidelines that recommenend annual magnetic resonance imaging (MRI), for women with certain genetic mutations and whose family history shows a high cancer risk. But MRI is very expensive.
It can cost $ 1,000 or more per scan and it also produces false positive results. Researchers at the Washington University in St. Louis (WUSTL) developed a new imaging scanner. They integrated thermoacoustic and photoacoustic tomography (TAT/PAT) to get a dual-contrast image. The low-cost scanner that detects microwave and light absorption may provide a non-ionizing and high-resolution,dual modality 3D image of the breast, the scientist explain in Medical Physics.
"Depending upon the clinical testing outcome, TAT/PAT could potentially replace X-ray mammography if its sensitivity and specificity are high enough," Lihong Wang, director of WUSTL's Optical Imaging Laboratory, told medicalphysicsweb. "Otherwise, it can serve as an adjunct.”
Two in one
TAT works by irradiating tissue with microwave or RF pulses. When this energy is absorbed, it causes localized heating that results in a pressure wave. This wave is detected by ultrasound transducers at the tissue surface and can be used to generate an image.
The RF contrast between malignant tumour tissue and normal human breast tissue is about 4:1, with one recent study showing a contrast in dielectric properties between malignant and normal adipose-dominated breast tissues of up to 10:1. In comparison, X-ray contrast is typically only a few percent among soft tissues.
PAT exploits the same effect, except that the ultrasound is generated by irradiating the region of interest with pulsed near-infrared light. Here, the image contrast arises from the degree of vascularization within the tissue, with the optical absorption contrast of oxy- and deoxyhaemoglobin relative to the background as high as 10:1. Thus PAT is ideal for quantifying features such as angiogenesis and hypoxia, which are correlates of breast malignancy.
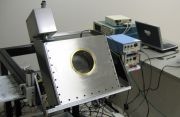
To create the dual-modality scanner, the WUSTL researchers integrated a 1064 nm Nd:YAG laser and a 3.0 GHz microwave source into a single device. The ultrasound signals are detected by transducers that revolve by 360 degrees around the sample. The breast is placed in a cylindrical aperture at the front of the scanner and compressed from the front, which potentially enables imaging near the chest wall. The system can instantaneously switch between microwave and laser illumination.
The researchers tested the TAT/PAT scanner using tissue phantoms made of porcine fat to mimic fatty breast tissue. Five water-based gel targets were buried inside the phantom - two made of clear gel and three of black gel.
The RF absorption contrast between the gel and the background fatty tissue is about 4:1. As expected, TAT clearly imaged all five targets. The contrast, signal-to-noise ratio and resolution in the reconstructed TAT images were around 3.5:1, 34 and 1.2 mm, respectively, for the 13-mm transducer, and about 2.5:1, 20 and 0.7 mm for the 6-mm transducer.The reconstructed PAT images only revealed the black targets, as the contrast in this case is dependent on light absorption. Here, the images exhibited contrast, signal-to-noise ratio and resolution of about 4.1:1, 64 and 0.7 mm, respectively, for the 13-mm transducer, and around 3.8:1, 27 and 0.7 mm for the 6-mm transducer
The researchers conclude that "TAT and PAT together can provide additional functional information for the diagnosis of breast cancer." Integrating the two modalities into a single system also enables consecutive image acquisition without having to realign the patient - reducing both scanning time and system cost.
04.07.2008
More on the subject: