Article • CSI
3-D printed hearts
The CSI Congress (Congenital, Structural and Valvular Interventions) is one of the major fixtures for catheter therapy of congenital and structural heart defects. Key moments in this high profile event are live broadcasts and the audience can not only to listen to but also interact with the teams in the cath labs involved.
Report: Ralf Mateblowski
To see the model means to change strategies.
Dr Sameer Gafoor
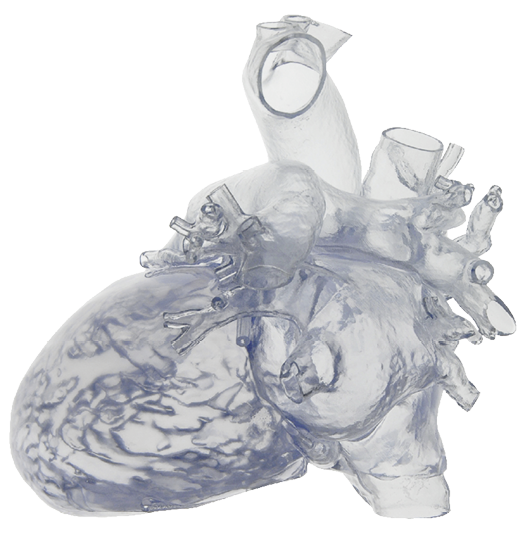
At last year’s CSI gathering, three live interventions – one case of mitral valve insufficiency, a degenerated bioprosthetic tricuspidal valve and a transcatheter aortic valve implantation, performed in Frankfurt/Germany in late June – demonstrated how patient-specific 3-D printed heart models can be used for surgical planning.
Belgium-based manufacturer Materialise offers software solutions and services for 3-D imaging and 3-D printing. Just before he began to enable the first live case, Dr Sameer Gafoor of the Cardio-Vascular Centre Frankfurt summarised his experiences with the firm’s HeartPrint models. ‘To see the model means to change strategies,’ he said.
Based on CT, MRI and/or 3-D ultrasound image data, the transparent silicone models show the individual anatomy in amazingly realistic detail. This allows a physician in the pre-operative planning phase to literally get his hands on the structures he is going to see – down to the different tissue thicknesses of muscles and vessels, including calcifications! This kind of haptic exploration of the intervention site helps to decide whether catheter access will in the leg or the neck. In turn, that decision informs the choice of instruments to be used. In complex cases, interventional cardiologists and cardiac-surgeons can test their actual operating theatre strategy on the model, adapt their procedure, if needed, and even discuss it prior to the intervention, during the multidisciplinary cardio board. Thus, the entire team knows what’s in store.
‘Basically open heart interventions cannot be repeated,’ Dr Gafoor explained, pointing at two further advantages of 3-D print models for planning purposes – high surgical success rates and markedly improved patient outcomes. Even more: the ‘test runs’ with the 3-D models reduce intervention time, which in turn has several positive side effects: shorter anaesthesia times reduce health risks for the patient resulting in faster recovery. For the hospital this translates into quicker theatre turn-around-times and shorter length of stay. In short: significant cost savings.
Basically open heart interventions cannot be repeated
Dr. Sameer Gafoor
3-D models are not only used for intervention planning, they also support patient information very effectively: now the patient may better understand why the intervention is necessary and how it is going to be done. This should deepen trust in the physician and intervention acceptance – an important psychological factor, positively impacting on a patient’s attitude before, during and after the intervention.
Obviously ‘learning by 3-D model’ is not limited to physicians, patients and families – it is also a perfect tool for training medical students and junior cardio-surgeons. Last, but not the least, the medical technology manufacturers benefit from 3-D models from the development, throughout pre-clinical trials to product marketing. While the use of 3-D models in cardiology, as described above, is more or less still in the beginning cranio-maxillofacial surgery and orthopaedic patients already receive 3-D printed implants. In these disciplines the innovation potential of 3-D print models to optimise patient-specific care is already being realised and the results indicate immense potential awaits exploration in cardiology – above all in paediatric patients, since a baby’s heart can be merely the size of a walnut.
Profile:
Dr. Sameer Gafoor is an attending physician at the CardioVascular Center (CVC) Frankfurt, headed by Horst Sievert, MD. He obtained his medical degree from Northwestern University in the United States, followed by Internal Medicine Residency at University of michigan. His cardiology training started with Cardiovascular Disease Fellowship at Washington Hospital Center/Georgetown University and continued with Interventional Cardiology Fellowship at Emory University. Following this training, he went on to complete an Advanced Fellowship in Neurovascular, Coronary, Structural Heart, and Peripheral Vascular Training at the CVC Frankfurt. He specializes in interventions and imaging for structural heart and peripheral vascular disease, as well as development and incorporation of new devices, technologies, and techniques for these and other indications.
18.02.2016