Article • DNA modification
CRISPR/Cas9 and Sherlock: Savers, healers or threats to life?
Modifying a DNA sequence to alter a cell to cure a disorder, prevent a genetic disease being passed on to next generations, or to use genetic modification as a way to diagnose a virus: yes, these tasks are possible. The recently discovered CRISPR technique can do it all.
Report: M van de Wouw
Already in 1987 researcher Yoshizumi Ishino, at Osaka University, described the possibility of genome editing. In 2012-2013 scientists discovered genetic modification of a specific DNA sequence in a cell and gave it the name CRISPR. The discovery was runner up in 2012 and 2013 in Science Magazine’s Breakthrough of the Year award. CRISPR won the award eventually in 2015. Largely due to its simplicity and adaptability the technique rapidly became one of the most popular approaches for genome engineering. And so the development goes on.

What is CRISPR/CAS9?
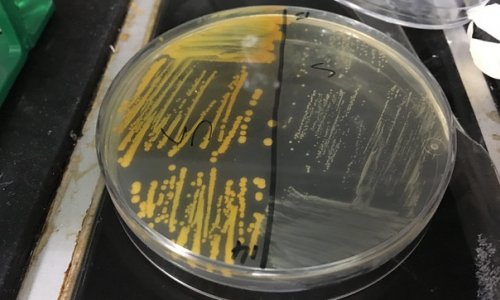
CRISPR is an abbreviation of Clustered Regularly Interspaced Short Palindromic Repeats. These short segments of repeated codes in DNA were first discovered in bacteria, where they play a key roll as part of the bacterial defence mechanism against viruses. So far, three distinct bacterial CRISPR systems, types I, II and III have been identified. The Type II system is the basis for genome engineering technology available at this moment.
Cas (CRISPR Associated System) is the name for different enzymes/proteins. Cas 9 is protein 9 and, together with CRISPR, is the basis for the technique used to edit the human genome. Cas9 is programmable and works in any type of cell.
How it works
CRISPR/Cas9 allows permanent modification of genes within organisms, therefore manipulating the code of life. It works like a pair of molecular scissors: when CRISPR is used to edit genes in a cell, a small strip of RNA directs an enzyme capable of cutting DNA at a desired location within a genome. This allows existing genes to be removed and/or new ones added. The cell recognises the damage done by the cut and ‘glues’ the pieces back together. And, although the cell is a bit shorter after the cut, it functions again.
Genome editing techniques have many potential applications, such as to target virulence factors, genes encoding antibiotic resistance, cancer, inflammation, foetal haemoglobin and even eradicate viral DNA in the case of Epstein-Barr virus (EBV). There are more than 3,000 genetic diseases, such as colour blindness or Huntington’s disease, caused by one wrongly placed nucleotide in the DNA.
CRISPR may even revive the concept of transplanting animal organs into humans. The biggest problems in transplant rejection are the retroviruses present in animal genomes. Researchers are working on eliminating those retroviruses DNA.
Ethical issues
OHSU scientists recently used CRISPR on a human embryo to correct a mutation in nuclear DNA that causes a common genetic heart disease, leading to sudden cardiac death and heart failure. By removing the disease-causing gene variant from the lineage, every future generation would carry the repair. It was a success. However, the potential to alter DNA in human cells needs more investigation, because it is still unknown what the long-term side effects will be. In future, potentially infected diseases may occur.
The use on human embryos also causes an ethical issue. How far should we go? Policy regulations for the CRISPR/cas9 system vary internationally. Researchers in China, Sweden and the United Kingdom are allowed to use human embryos for CRISPR interventions, although in the UK it is forbidden to implant the embryos. They must be destroyed after seven days. The Netherlands does not permit the use of human embryos. According to some, the potential danger in the long run is the temptation to treat children not only for genetic disorders but also to make them perfect: superior intelligence, better eyes, and better muscles. Rules for applying CRISPR/Cas9 are therefore necessary.
Sherlock
Besides being able to repair DNA, CRISPR could soon also become a low-cost diagnostic tool to detect infectious diseases such as Zika or dengue. According to a recent article published in Science researchers have developed the Specific High-sensitivity Enzymatic Reporter (SHERLOCK), which stands for ‘to make accurate, fast diagnoses’. This uses a different enzyme, Cas13a, which goes to RNA, rather than DNA. It chops through any RNA encountered and does not stop until that has gone.
The development of Sherlock gave medical laboratories a new diagnostic tool. And the scientific community is excited. Sherlock can detect pathogens in extremely small amounts of genetic matter and in an earlier stage. Besides that, tests can be performed using urine and/or saliva rather than blood. Quoted from Science: ‘The detection sensitivity of the new CRISPR-Cas13a system for specific genetic material is one million times better than the most commonly used diagnostic technique’. The technique is also highly portable, needs no refrigeration and costs as little as 61 cents per test in the field. Therefore Sherlock would be extremely useful in remote places without electricity or access to a diagnostic laboratory, providing clinicians the possibility to diagnose and treat illnesses.
CRISPR/Cas9 and Sherlock can change and save lives. Professor and Director Scott Weaver PhD, at the Institute for Human Infections and Immunity, University of Texas Medical Branch in Galveston, states in an article on Big Think: ‘It looks like one significant step on the pathway that is the Holy Grail, which is developing point-of-care, or bedside detection, that doesn’t require expensive equipment or even reliable power.’
Source: https://www.washingtonpost.com/news/speaking-of-science/wp/2015/12/01/historic-summit-on-gene-editing-and-designer-babies-convenes-in-washington/?utm_term=.765ca64aafaf
http://science.sciencemag.org/content/356/6336/438
27.09.2017