Article • Imaging Infections
Zika birth defects decrease, but…
ECR 2017 Guest Lecturer Maria de Fatima Vasco Aragao, a radiologist from Pernambuco state, Brazil, has been tracking the Zika virus ever since it broke out in her country in 2015. She will highlight how CT and MRI can help reach diagnosis, especially in the absence of microcephaly. In an exclusive interview with European Hospital correspondent Mélisande Rouger, the radiologist warned there might be more to come regarding the spectrum of Zika syndrome, with possible outcomes such as epilepsy and cognitive impairment.

‘We do not follow patients routinely in order to prevent sedation of infants and ionising radiation. Control studies are only indicated after identification of clinical signs of a complication, for instance hydrocephalus and seizures. ‘Microcephaly and brain malformations can be diagnosed with ultrasound during pregnancy.’
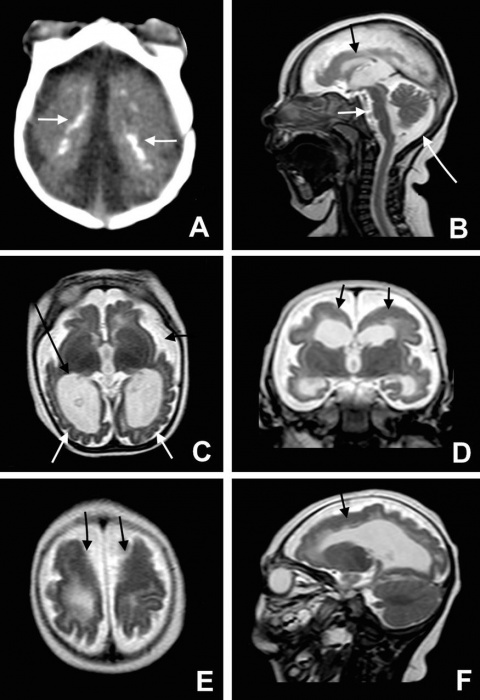
‘When a baby is born with microcephaly in an epidemic area, the paediatrician and neuropaediatrician usually suspect congenital Zika syndrome, whether or not the mother recalls a rash during pregnancy. But we are beginning to see cases in which neuropaediatricians don’t suspect congenital Zika syndrome, because the babies don’t have microcephaly, but have.normal-size heads.’ They undergo MRI examination due to unspecific neurological signs, e.g. delayed neuropsychomotor development and motor deficits. Here, radiologists must be alert, as the indication is not Zika virus or microcephaly, and microcalcifications may be subtle, so could be missed. ‘Not only the presence of calcification, but also its location at the cortical subcortical white matter junction needs to be identified, as it is highly suggestive of congenital Zika syndrome.
‘Another suggestive finding is malformation of cortical development predominant in the frontal lobes. In addition, these children are around one year and, therefore, specific IgM test for Zika virus can be negative, even if the child has the disease. Therefore, the radiologist’s responsibility is even more important in case of congenital Zika syndrome without microcephaly, to suggest the diagnosis to the paediatrician and neuropaediatrician.
In these cases, radiology is the only tool we have to make the diagnosis. So radiologists must be alert. ‘
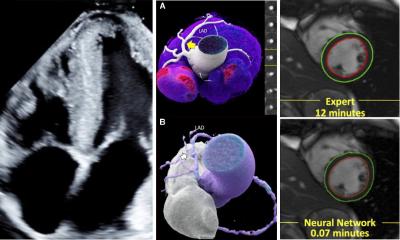
‘Imaging is important, especially in less severe cases, for early detection of congenital Zika syndrome, allowing rehabilitation to start quickly, to help improve their development. If microcephaly is absent and clinical signs appear when infants are several months old, the most important way to diagnose the syndrome is through imaging studies, so radiologists need to detect microcalcifications at the cortical subcortical white matter junction, which can be difficult on MRI, and malformations of cortical development, predominant in the frontal lobes.
‘Imaging is also important in identifying complications of the disease, such as hydrocephalus, in which the indication for surgery for ventricular derivation is important, to prevent neurological deterioration.’
How many cases are there?
‘Since its peak in October/November 2015, new cases of congenital Zika syndrome decreased throughout 2016. Two possible explanations: t the population is gradually becoming immune to the virus in north-east Brazil and prevention has become more intense, with people knowing how to protect against the Aedes aegypti, the mosquito responsible for Zika infections..
‘The WHO revealed that, as of 14 December 2016, 75 countries and territories, especially in Latin America, reported evidence of mosquito-borne Zika virus transmission. Up to then 29 countries, particularly in Latin America, had reported microcephaly and other central nervous system malformations; four were without endemic transmission. After Brazil, Colombia (67) and the USA (37) had most cases.’
Observational studies to understand the spectrum of this syndrome onginud. ‘The fact that some children do not present with microcephaly but image alterations raises questions of great importance for public health. Perhaps we’ve seen the tip of the iceberg with the most severe brain damage cases associated with microcephaly.‘ Researchers want to know the real size of what is submerged, where minor changes without microcephaly could cause future problems, e.g. epilepsy and cognitive impairment..
‘Other groups are trying to evaluate prospectively the risk of developing microcephaly and other abnormalities after Zika infection during pregnancy. Besides congenital microcephaly, neurologic complications have been found in adults.’ According to the WHO, up to 14 December there was an increase in Guillain-Barre cases and/or laboratory confirmation of Zika virus infection among Guillain-Barre cases in 20 countries. Myelitis and encephalitis have also been identified. ‘As radiologists, we try to help the scientific community to understand the pathophysiological process of the disease.’
Is there hope of a treatment?
‘There is neither specific treatment nor a vaccine. Although vaccination can be developed, a treatment for the lesions caused by the virus is extremely unlikely. This does not mean there is nothing to do. Once the disease is recognised, rehabilitation must begin immediately, especially in less severe cases, to provide the chance of better neuro-psychomotor development for the children and support for their families.
‘Treatment and support must also be directed towards other disease manifestations, – seizure, ophthalmologic and auditory deficits, arthrogryposis and possible complications, e.g. hydrocephaly.’
PROFILE:
Radiologist Maria de Fátima Viana Vasco Aragão is president of Pernambuco Radiology Society, professor of radiology at the Maurício de Nassau University and Scientific Director of the Multimagem Diagnostic Centre in Recife.
Event information:
GL - Breaking News from Latin America
Wednesday, March 1, 12:15 - 12:45
Room: B
Session Type: Headline Sessions
Topic: General Radiology
01.03.2017