Article • POCT as initial coronavirus screening tool
Ultrasound confirms frontline value in COVID-19 setting
Ultrasound could become the prime modality in emergency settings for tracking disease progression in COVID-19 patients.
Report: Mark Nicholls
While chest CT has held a key diagnostic role thus far, many experts now advocate the benefits of ultrasound within the context of the coronavirus epidemic. Dr Rachel Liu, who recently led a high-profile panel discussion with experts from the USA and areas of Europe with high incidence of COVID-19, discussed the advantages offered by ultrasound, and particularly point-of-care ultrasound (POCUS).

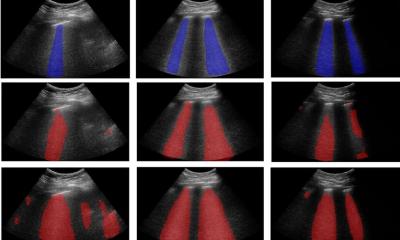
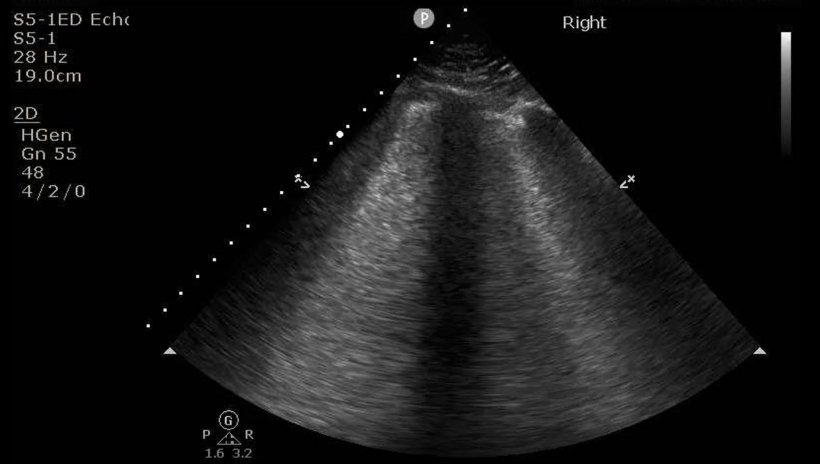
Liu believes the role of POCUS and traditional ultrasound has changed with the length of the pandemic, and will continue to evolve. ‘In the early stages of the crisis, lung ultrasound was used diagnostically in conjunction with COVID swab testing, because swab testing could be unreliable,’ she explained. ‘It may have also been used to aid physicians in selecting the patients most eligible for swab testing.’ However, as the pandemic evolved, and with better testing available, the value of ultrasound as a portable, flexible and time-efficient modality increased, with its value becoming more apparent in categorising mild, moderate or severe disease, discharge decision-making, and baseline monitoring of cardiac function and lung involvement for patients admitted to the hospital, for example.
Liu, who is the emergency ultrasound fellowship director for the Department of Emergency Medicine and the Director of Point-of-Care Ultrasound Education for Yale School of Medicine, said the key seasons ultrasound has emerged as a first liner in emergency settings to diagnose COVID-19 is largely due to avoidance of exposure and transmission of virus particles; disinfection; and preservation of PPE. ‘Emergency personnel are often the first to see, examine, and talk to a patient,’ she said. ‘As we need to see the patient anyway, it makes sense if we perform as complete an evaluation as possible to avoid others needing to come into contact with that patient. This includes obtaining swabs, lab work and imaging. If the emergency provider can perform diagnostic imaging at the same time as evaluating the patient, then this prevents others – transporters, cardiologists, radiologists and technicians – from needing to come into close contact with the patient.’
A second critical area is cleaning and disinfection, particularly where CT suites are fixed spaces that would be shared by COVID and non-COVID patients. ‘Many hospitals do not have enough machines, or the infrastructure to create cohorted radiology spaces. So, a CT performed on a COVID-positive patient would shut down that machine for up to an hour, so that it, and the surrounding space, can be cleaned. Contrast that with a portable ultrasound machine which can be cleaned and disinfected in a matter of minutes, with a dwell time of only 2-3 minutes between cleaning and use on the next patient. Often, and particularly if a site also uses pocket or handheld devices, there is more than one machine in the emergency department. That means that there is a possibility of dedicating machines solely for use in COVID spaces, while also having machines available for non-COVID spaces.’ Thirdly, as fewer people need to come into contact with the patient, less PPE is used, which helps conserve PPE in a time of worldwide shortage.
Liu said ultrasound offers advantages over CT, and other modalities, in the coronavirus context and points to preliminary literature in the COVID time period, as well as previous imaging literature on Acute Respiratory Distress Syndrome (ARDS), suggesting that lung ultrasound approaches share similar test characteristics with CT. With all the advantages of isolation from others, speed of operation and cleaning, Liu concluded POCUS to be overall ‘the most expedient modality’. Portable chest X-ray, she added, does not have test characteristics that match CT, and findings on both CT and lung ultrasound can be seen before they appear on X-ray, though she acknowledged that all imaging has limitations.
5 reasons for diagnostic ultrasound
Prior publications on ultrasound in H1N1 and ebola patient care already suggested this, but this pandemic has really made this concept hit home
Rachel Liu
The 10-strong expert panel’s discussion report highlighted five reasons why diagnostic ultrasound should be considered for imaging in suspected COVID infection cases: both a normal and abnormal lung ultrasound may provide key clinical insights; lung ultrasound may help rule out other pulmonary diseases; cardiac ultrasound could detect heart problems caused, or exacerbated, by COVID-19; ultrasound may benefit critically ill patients needing peripheral or central venous access; POCUS can reduce numbers of healthcare workers exposed while supplying immediate diagnostic information.
‘Much is still being developed,’ Liu concluded, ‘but I think the role of point-of-care ultrasound as an initial screening tool has become more established. Prior publications on ultrasound in H1N1 and ebola patient care already suggested this, but this pandemic has really made this concept hit home. This can translate to imaging considerations throughout the length of the pandemic, as well as in future pandemics. Because of this, POCUS should be firmly established in future emergency preparedness and global public health or public policy plans.’
Research is underway in developing severity scores based on ultrasound findings, Liu added, and this may help in the second or third waves of COVID, as well as in future pandemics.
Profile:
At Yale School of Medicine, in Connecticut, Dr Rachel Liu is the emergency ultrasound fellowship director at the Department of Emergency Medicine and the Director of Point-of-Care Ultrasound Education. Her research interests include the use of point-of-care echo to guide performance of cardiopulmonary resuscitation, integration of new technologies into hospital and educational infrastructure, and system-wide development of point of care ultrasound programs. She has held all major leadership positions within the ultrasound sections of the American Emergency Medicine societies, notably the American College of Emergency Physicians, for whom she authored guidelines for implementation of handheld ultrasound technologies.
23.09.2020