To pulse or not to pulse
Whether mechanical, temporary cardiac assist systems should pulsate in the same way as a biological heart is a discussion topic, which raises the pulse rates amongst all those involved within the industry and in hospitals.
It happened in Orlando, Florida on 14 November 2011: Dr Timothy J. Gardner, Medical Director of Christiana Care’s Centres for Heart and Vascular Health and Past President of the American Heart Association, reignited the debate surrounding pulsing after around two decades of relative calm on this topic. Gardner talked about the development of a synchronised cardiac assist device.
This would be as small as an ICD and was to detect the patient’s ECG signal. Connected to the subclavian artery, it was going to generate a stroke volume of 30 cc – in the counter-pulsation known from the IABP. That was predicted to take the strain off the heart, improve coronary circulation and improve the supply of the peripheral organs.
One weak point was the limited frequency: The device only pulses to 100 bpm; above that it would pulse continuously and the physiological advantage would be gone. However, Gardner encouraged everyone to trial the device and amongst ‘plenty of good reasons’ included the ‘current need for an activity-friendly IABP’. At the end of January 2012, again in Florida – but now in Fort Lauderdale – Dr Renzo Cecere, Director of the Mechanical Assist Programme at McGill University Health Centre in Montreal, Quebec, reported on his first two implantations of the new assist devices in humans. He was pleased with the recovery potential, which the new product from Abiomed called Symphony offered for 28 days up to the point of its scheduled explantation, and expressed hope that the comparatively simple intervention would soon make it possible to not only treat patients with congestive heart failure with a conventional LVAD at the therapy-refractory terminal stage when they no longer respond to medication, but to slow down the progress of the disease at a relatively early point, thus significantly increasing quality of life.
‘The concept of a minimally invasive implantable pump for patients in chronic heart failure, coupled with the ability to remodel the heart, is unique and ground-breaking, and we are very pleased with the initial findings of Symphony,’ said Cecere.
From the USA to Germany
Although this study is not yet finished, contrary to the initial plans, another pulsatile cardiac assist device was recently trialled in Germany for the first time. On 25 June, his 56th birthday, Kurt-Josef M. was the first patient worldwide to have the Heartmate III by Thoratec implanted at Hanover Medical School.
One of the innovations of this type of device is an artificial pulse. To achieve this, the revolutions of the pump are slowed down and then sped up again every two seconds. However, this does not work under stress. ‘We can’t yet do this ECG-triggered,’ explains Dr Jan Schmitto, who implanted the device. It is also not yet quite clear what the optimum pulse frequency should be. Whether a pulse beat is even necessary is currently the subject of scientific discussion.
Schmitto cites physiological arguments: ‘In older patients in particular we may be able to reduce complications from gastrointestinal bleeding in the long term by generating a little pulsatility.’ Moreover, with a lacking pulse there is a danger that the media, the muscular layer of cells in the arteries, atrophies if it is no longer activated – which probably increases the risk of capillary ruptures in the gastrointestinal tract.
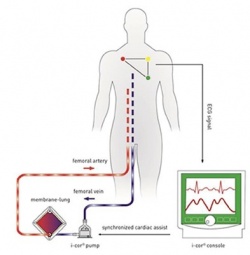
Around three months before (25 March 2014), Dr Ulrich Laufs, Professor for Clinical-Experimental Medicine at Saarland University in Homburg, had given a much-regarded lecture. Using the i-cor manufactured by Novalung, the first pulsatile circulatory assist device for interventional cardiology (image) which actively pumps blood, he managed to measure coronary flow, which was around 300% higher than conventional, non-pulsatile perfusion in animal experiments (n=8) with a fibrillating pig heart. As the device also has an ECG trigger, this makes heart-synchronic extracorporeal circulation with diastolic augmentation possible.
It also eliminates the main disadvantage of conventional extracorporeal life support (ECLS): the bloodstream is no longer continuously pumped against the weakened heart. This lowers the cardiac afterload and the need for oxygen. At the same time, coronary perfusion increases and therefore the amount of oxygen available. Last, but not least, the circulation in the end organs improves – as Timothy Gardner put it, ‘plenty of good reasons’ for the i-cor, which can even pulsate up to a heart frequency of 150 bpm.
02.09.2014