The pulseless life
by Holger Zorn
New pulsatile heart pumps (ventricular assist devices - VAD) can remain in the body as a permanent heart support.

Tubes the thickness of a thumb transport blood from the heart through the diaphragm, the abdomen and abdominal wall into the artificial pumping chambers - powered by vacuum and compressed air - then back to the lung artery or the aorta. Such paracorporeal systems can support the left, right or even both ventricles. However, life with these systems is not particularly comfortable: Four tubes guided through the abdominal wall mean four entry ports for pathogens; moreover, the compressor and many batteries must be carried along always. Although individual patients have been supported in this way for over three years, and longer, the use is generally limited to a few weeks or a few months – until such a time when a suitable donor heart can be implanted (bridge to transplant - BTT).
However, over the last few years, the number of donor hearts, at least in Europe, has been on a continuous decrease. The Eurotransplant International Foundation, responsible for the mediation and allocation of organ donation procedures in Austria, Belgium, Germany, Luxembourg, The Netherlands, Slovenia and (as a candidate) Croatia, reports a mere 530 heart transplants in 2005; another 864 patients are on the waiting list, 720 of these in Germany. 352 hearts were transplanted between January to August this year - six less than in the same 2005 period. This continuous gap between requirements and availability of donor hearts (see fig. 1), has significantly promoted the development of implantable, mechanical blood pumps.
Real artificial hearts (TAH), which are implanted into the chest cavity, are comparatively rare. First, they also require external power; second, implantation is surgically considerably more complicated; third, a heart that has been supported by a VAD for a period of time can sometimes recover to such an extent that the device can be removed again – obviously not possible with a total heart replacement.
This hope for organ recovery (bridge to recovery - BTR) has increased the acceptance of mechanical heart pumps and promoted the development of smaller, lighter and long-term stable systems. They no longer utilise the principle of displaced volume but that of the Archimedean screw, i.e. they continuously pump blood from ventricle to artery – blood pressure can no longer be measured in the conventional way. One of the pioneers of mechanical heart support use, cardiac surgeon Ernst Wolner, in Vienna, calls this the ‘pulseless life’. Such axial pumps are installed in the chest cavity; only a controller cable is guided through the abdominal wall to the outside and connected with the controller and batteries. They have been designed to assist the left heart ventricle (left ventricular assist device - LVAD); this should be left with a certain amount of its own functionality – at least 10%. The right heart works by itself. Contained in a pod in the blood stream, the propellers are practically free from wear, pump between 3-9 litres of blood per minute, at between 8,000-18,000 rotations and do not require more anticoagulation than an artificial heart valve.
This operational performance has encouraged engineers and convinced investors to develop a new generation of LVADs: Centrifugal pumps that work without any mechanical bearings and are powered by a magnetic field. The centrifuges pump the same amount of blood with a significantly reduced rotational speed and better adapt to differing requirements of the organ – e.g. high physical pressure during sport. There is less pressure on the material, the pumps – it is expected – will remain in a patient for longer and an alternative to heart transplantation is within sight: a so-called ‘destination therapy’ (DT) that should be more appropriately called ‘lifetime therapy’.
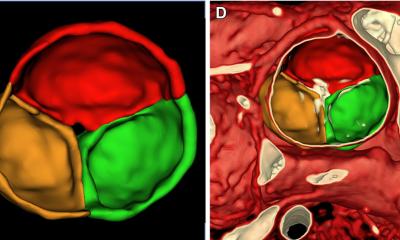
At the 14th Congress of the International Society for Rotary Blood Pumps (ISRBP) held in Leuven, Belgium (31/8 to 2/9), six centrifugal pumps were introduced (fig. 2) to facilitate this lifetime therapy. Although all are ready for use, they vary in their developmental stages; this ranges from two (Rotary VAD) and three (EvaHeart) to 65 (VentrAssist) clinical uses. The most advanced, the Ventracor system (pic. 1) is expected to receive its CE mark at the beginning of 2007 – the commencement of its marketing in Europe. During the licensing study (BTT) 30 patients, aged 10-66 years, were involved. 25 patients (83.4%) lasted to the end point of the study (defined as transplant or 154 days supported by the system and still suitable to receive a transplant), four died, one recovered to such an extent that the system could be removed again. The median time of support was 167 days. There were five reported strokes or 0.36 events per patients year. In all 65 patients the accumulated patient experience was 33.3 years; the longest support period: 977 days.
For comparison: Novacor LVAS by WorldHeart, the pulsatile left heart support system was first successfully implanted in 1984 and, to date, has supported more than 1,700 patients. Jack Fawbush of Whitesburg, Tennessee, USA, has lived with the system since July 2001, i.e. over five years. From his 67th year, Peter Houghton of Oxford, UK, has lived with the support of the Jarvik 2000 (Jarvik Heart Inc. New York, NY, USA) for six years, and he has devoted the extra years of life, made possible by the support of this system, to promoting the use of, and information about artificial heart pumps. Encouraging stories, which lead us to hope for more: more patients with more life. Ventracor wants to prove this: ‘We recognize wide market acceptance needs more than regulatory approval, so have started the Baseline Results and Cost Effectiveness (BRACE) Study in Europe,’ said CEO Peter Crosby during the European Cardiac Surgery Congress, held in Stockholm this September. The study is clearly aimed at patient success – and therefore very simple: Is the patient still alive after two years and if so with what quality of life and what treatment costs?
It will be hard to show this as the bar has been raised. Dr Martin Strüber, cardiac surgeon at the Medical University Hanover, Germany, pointed out: ‘There are enough good assist devices for bridge-to-transplant, but what we need is a good device for destination therapy.’ He added that progress in pharmacotherapy or biventricular pacing only increase quality of life for limited periods of time, but overall they increase the waiting list for donor hearts – or an LVAD. In Leuven, Dr Strüber presented data on HeartMate II (Thoratec Corp., Pleasanton, CA, USA), a VAD (pic. 2) first implanted on 20 November 2003 at the Texas Heart Institute by Dr Frazier. The pilot study involved 46 patients (22 from Europe; 24 the USA) aged between 14 and 69 years. The longest support period was 863 days; the median 256 days. 16 patients were supported for over a year, ten for over 1.5 years and four patients for over two years. Three strokes and three transient ischaemic attacks (TIA) were observed – an equivalent of 0.11 events per patients year. The CE mark was awarded in November 2005 and, since then, over 470 systems have been implanted (100 in Europe). ‘On average we carry out at least one implantation a day,’ said Martin Muller, hospital co-ordinator at Thoratec.
Whereas a similar system, manufactured by a German company, has so far only achieved good results when handled by renowned specialists – and axial pumps manufactured by other firms only lead a niche existence – the HeartMate II can be considered a benchmark. All new technologies, all new equipment will have to prove their results are at least as good. That all six manufacturers will survive in this market is unlikely. Just two or three might. This field, particularly in Europe with its ageing population, is on the brink of a breakthrough: If current results can be reproduced, patients with mechanical heart support systems will no longer be considered exotic in a few years time. Soon the whole spectrum of products will be available: The Lifebridge (see European Hospital 3/2005) can be used for several hours for the safe transport of patients in cardiogenic shock. A severely damaged heart that still has sufficient tactile tissue can re relieved with micro-axial pumps of the type Impella (Impella CardioSystems GmbH, Aachen, Germany) for 10 days, or with the centrifugal pump Centrimag (Levitronix AG, Zurich, Switzerland) for 14 days, to an extent that it will either recover or can then be fitted with a long time assist device. This short-term therapy actually could be considered clinically established. For example, Impella pumps have been used in 17 European countries and 140 hospitals 745 times (154 in Italy) since their inaugural implantation on 30 March 1999. This development is fascinating for many: The Cleveland Clinic (Cleveland, Ohio, USA) is currently developing a pump with magnetic bearings for use in paediatrics. Turkish researchers at Yeditepe University, Istanbul, have introduced the prototype of the micro axial pump ‘Heart Turcica-1’. CircuLite Inc. (Hackensack, NJ, USA, and Aachen, Germany) has introduced a product of the same name (pic. 3) that can be implanted without the use of a heart lung machine. Inserted into the chest cavity via a small cut between two ribs, it is connected via the superior vena cava trans-septally to the left atrium (inflow side) and to the arteria subclavia (outflow side) and then pumps 2-3 litres per minute. The development’s objective is to get the patients earlier and less sick – and finally to achieve catheter-supported implantation by interventional cardiologists, to weaken their scepticism about all forms of mechanical heart support and to send more patients to cardiac surgeons – patients who are currently still kept from them.
17.11.2006