Image source: Regenstrief Institute
News • Standardisation in healthcare
Study surveys landscape of FHIR apps
A new study led by Regenstrief Institute Research Scientist Titus K. Schleyer, DMD, PhD, is among the first to survey the current landscape of FHIR apps, providing a snapshot of how the standard is used to enable the flow of health information.
FHIR might seem like an obscure technical concept, but it has everyday applications and uses for patients, for clinicians and for healthcare systems
Titus Schleyer
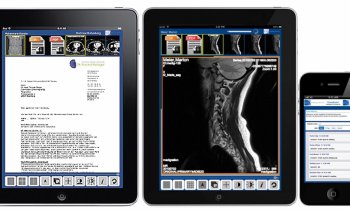
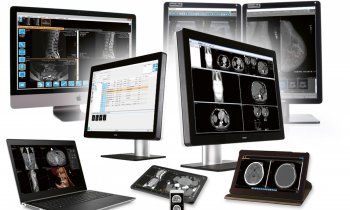
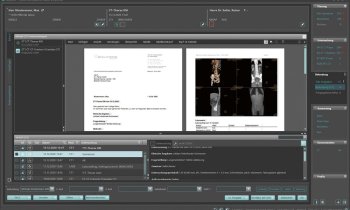
FHIR apps can pull in data from most electronic health record systems, facilitating secure movement of information when and where needed. FHIR, pronounced ‘fire’ and short for Fast Healthcare Interoperability Resources, standardizes how healthcare information is exchanged between different computer systems regardless of how it is stored in these systems. FHIR apps consume information through the FHIR interface. The global interoperability standard can be used for exchanging health data between physicians and patients, as well as among clinicians and healthcare systems. “FHIR might seem like an obscure technical concept, but it has everyday applications and uses for patients, for clinicians and for healthcare systems. It makes health information more accessible, not just among clinicians, but also clinicians and patients,” said Dr. Schleyer. “In fact, the core asset of many FHIR apps is to take information out of an electronic health record and do useful things with it, such as identify trends, provide clinical decision support or handle a niche area not covered by a commercial electronic medical record system.”
Recommended article

Article • Health IT
Interoperability: Insights from Down Under
With interoperability stalled, stakeholders are seeking new ways to create an interoperable ecosystem. IT specialist Jason Steen describes the state of interoperability in Australia and calls for more governmental commitment and international standards.
“Publication of this broadly collaborative work represents a critical step in emphasizing the important global effort toward the implementation of HL7 FHIR,” explained Charles Jaffe, M.D., PhD, a co-author on this study. “As the adoption of FHIR for patient care and research becomes more ubiquitous, we look to this platform as an important resource for the expanding community of end-users as well as technical implementers.” Dr. Jaffe is chief executive officer of HL7. The new study, published in JAMIA Open, notes the rapid development and adoption of free and easy-to-use FHIR apps over less than a decade and forecasts accelerated development and use of these apps in the future.
To assess the landscape of FHIR apps, 112 were studied. A total of 74 were focused on clinical care and 45 on research. The majority were standalone and web-based with a smaller number embedded within an electronic health record. Most of the clinical apps were implemented across multiple healthcare settings, highlighting, according to the authors, the easily substitutable nature of FHIR. Most apps were developed by software vendors and were targeted at health professionals, rather than patients. “When we talk about FHIR, we are talking about an innovative way to securely share health information from different information systems,” said Dr. Schleyer. “You can think of FHIR as a ‘plug and play’ standard, very similar to the electrical plug used in your home. When we plug a device into an outlet, electricity flows and then the TV or other device comes to life without us having to worry about what the plug does. It’s the same with FHIR. Information across systems can be accessed using this innovative standard.”
In the U.S., patient-facing FHIR apps are a requirement for electronic health record certification in accordance with the 21st Century Cures Act. In 2023, the Centers for Medicare and Medicaid Services (CMS) will begin requiring payers to implement FHIR apps for various use cases. The European Union’s InteropEHRate and India’s Digital Health Blueprint focus on implementing FHIR-based personal health records and data sharing with providers. New Zealand’s Ministry of Health and the United Kingdom’s National Health Service provide access to national patient identifier systems using FHIR.
Source: Regenstrief Institute
05.01.2023