Safire: The world's first direct-conversion R/F-FPD
Dr Hiroyasu Yano reports on the effective use of tomosynthesis in orthopaedic surgery.
Due to looseness of the stem, 11 years after bilateral total hip replacement surgery the left joint was replaced in a 73-year-old female.
The bilateral hip replacement post-surgical CT image in Fig.1 b) includes significant artifacts due to the implant between the acetabulum and trochanter. The shift-and-add method image in Fig.1 c) exhibits no effects of artifacts, whereas the FBP image in Fig.1 d) exhibits artifacts in the tube-shift direction and at the boundary of the implant.
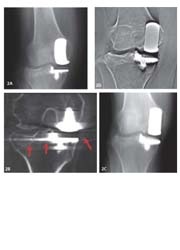
Fig. 2: Fracture after knee replacement
A 59-year-old female, who had undergone knee replacement surgery due to osteo-arthritis, fractured the lateral tibial plateau in a fall. The CT image in Fig.2 b) exhibits effects of the implant artifacts to the lateral side of the tibia. However, these effects do not extend to the lateral side in the shift and add method image or the FBP image (Fig.2 c, 2 d).
The 52-bed, acute care Hachiya Orthopaedic Hospital conducts 330 surgical operations annually, including minimally invasive artificial joint surgery and endoscopic surgery. In 1996, the hospital digitised ordering; in 1998, imaging was digitised; in 2004, a urology department was added.
During orthopaedic surgery, metal implants, plates, and screws are commonly employed. These frequently cause problems with metal artefacts during CT or MRI examinations of bone union and in post-surgical follow-up observations. This is a report on the use of tomosynthesis to restrict metal artifacts in images.
Current tomosynthesis status: Since introducing the flat-panel detector (FPD) in 2005, we have conducted tomosynthesis examinations on 35 artificial joint cases (20 hip, 10 knee, 5 elbow), 8 spondylodesis cases, 3 arthrodesis cases, and 4 osteosynthesis cases.
Evaluation as clinical images: Tomosynthesis images created by the shift-and-add method and filtered back projection (FBP) method were compared with CT images. For this we used the Shimadzu Sonialvision Safire* R/F system with Tomosynthesis Workstation option and the MSCT: Company A, 6-slice CT.
Evaluation of the bone union of the grafted bone is based on the continuity between the grafted bone and original bone, and on the reduction in radiolucent lines. As doctors found evaluation difficult due to the strong enhancement of the FBP image in Fig.3 d), subsequently the shift-and-add method image in Fig.3 c1) was used. The shift-and-add method image in Fig.3 c2) was taken 14 months after surgery. It shows that bone union is almost complete.
Conclusions
Fig.4 compares CT and tomosynthesis images. For a CT examination in which radiography is conducted while rotating the body axis, the significant metal artifacts centred on the metal, and the beam hardening occurring between metals, affect the raw images. Blurring occurs along the path of the X-ray tube during tomography. However, as the images are two-dimensional, the effects of the artifacts are less than with CT. Low-artifact images can be achieved by selecting shift-and-add method images or FBP images according to the aim of the examination.
CT is superior in some aspects, as it allows flexible image reconstruction and produces 3-D images. However, due to concerns about X-ray exposure from radiodiagnosis since the publication of a paper in the Lancet in 2004 (A Berrington de Gozaiez, S Darby: Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet 363: 345-351, 2004), CT examinations have been classified in the highest exposure class of all radiodiagnostic techniques, with a tissue- absorbed dose between 10 and 100 mGy (T Ishiguchi: Risk Management in Radiology, Nichi-Doku Iryo, Vol. 31 - 3849, 2004).
As tomosynthesis requires fewer images than CT, the exposure dose should be lower.
Examining these topics and efficiently applying digital image technologies to take even better images in the future should make tomosynthesis an effective means of post-operative follow-up.
* Safire = Shimadzu Advanced Flat Imaging Receptor
01.03.2008