News • Suggestion for double reading practice
Solving the radiologist shortage with trained radiographers
When double reading screening mammograms, radiographers trained for the task perform as well as radiologists in key areas, according to a new publication.
Image source: University of Nottingham
The study was published in Radiology.
Double reading is the standard of care throughout Europe and it has been shown to improve cancer detection rates while simultaneously keeping recall rates low. The National Health Service Breast Screening Program (NHSBSP) in the United Kingdom has over 80 screening centers in England, where over 2 million women are screened annually.
To mitigate the strains put on the health care system due to increased workload and radiologist shortages, the NHSBSP has been using non-radiologists as part of double reading since the 1990s. While the traditional role of radiographers is to perform the mammogram, the NHSBSP recruits radiographers who undergo extensive additional postgraduate training to interpret the mammograms. They also participate in the same quality assurance standards as radiologists. “With the production of reliable individual reader performance data in recent years, it has been possible to produce a robust comparison of the performance of our radiologist and non-radiologist readers in England,” said study lead author Yan Chen, PhD, associate professor of cancer screening at the University of Nottingham School of Medicine in the UK.
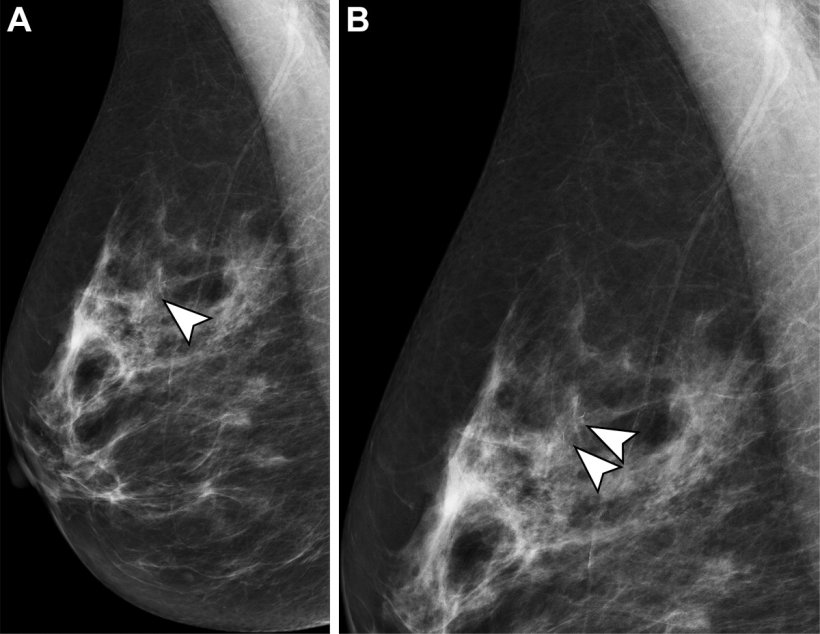
Image source: Chen et al., Radiology 2022 (CC BY 4.0)
For this study, researchers analyzed a year’s worth of performance data collected from 224 radiologists and 177 radiographers from the NHSBSP. Readers who also took part in the External Quality Assurance (EQA) scheme known as the Personal Performance in Mammographic Screening (PERFORMS) were eligible for this study and they also gave consent for their individual real-life breast screening performance data to be accessed from the Breast Screening Information System. Performance metrics that were analyzed were cancer detection rate, recall rate and positive predictive value of recall based on biopsy-proven pathological findings. Positive predictive value reflects the percentage of cancers found among exams for which biopsy was recommended or performed. Each metric was analyzed according to the reader profession, years of experience and any interaction between them using analysis of variance. Analysis of variance is a statistical formula used to compare variances across the means of different groups.
Researchers found no significant difference in the performance of readers from either professional group. The cancer detection rate for radiologists was 7.84 per 1,000 examinations, while the cancer detection rate for radiographers was 7.53 per 1,000 examinations. Additionally, the average recall rate for radiologists and radiographers was 5% and 5.2%, respectively. The final performance metric, positive predictive value of recall, also showed no variation. The positive predictive value of recall was 17.1% for radiologists and 16.1% for radiographers.
The outcomes of this study may lead screening programs in other countries to consider the use of physician extenders in breast imaging
Yan Chen
“It has been really gratifying to show that there was little difference in the performance of readers from either professional group when we looked at the key breast cancer screening performance metrics of cancer detection rates, recall rates and positive predictive value of recall,” said coauthor Jonathan J. James, FRCR, consultant radiologist and director of education and training at the Nottingham Breast Institute at Nottingham University Hospitals NHS Trust.
The results of this study also showed that reading performance was based on the years of experience of the readers. This suggests that appropriate focused training, participation in EQA schemes like PERFORMS, and experience are all factors that contribute to the performance of a reader. “Many countries are experiencing a shortage of radiologists, and this is compounded by increasing demands and growing screening backlogs,” Dr. Chen said. “The outcomes of this study may lead screening programs in other countries to consider the use of physician extenders in breast imaging.”
In a related editorial, Regina J. Hooley, MD, professor of radiology and biomedical imaging and vice chair for clinical affairs, and Melissa A. Durand, MD, associate professor of radiology and biomedical imaging, both from the Yale School of Medicine in New Haven, CT, acknowledge the potential value of physician extenders in mitigating the screening mammography workload without compromising patient care.
The authors also note, however, that physician extenders may not necessarily be an immediate solution to radiologist burnout. “Establishing a physician extender program in the United States and other similarly situation countries would require time and resources to develop appropriate training, certification, and ongoing professional development programs.”
Source: Radiological Society of North America
14.09.2022