Radiation exposure from cardiac CT - setting the record straight
By U. Joseph Schoepf MD FAHA, Professor of Radiology and Medicine and Director of Cardiovascular Imaging at the Medical University of South Carolina, Charleston, USA
Recent reports on cancer risk from radiation at CT have sparked new concern and discussion in the medical community as well as in the general public. It has been suggested that CT may be responsible for up to 2% of all cancers.


At coronary CT angiography using retrospective ECG-gating the effective dose to a 70 kg adult is estimated at ~ 12-20 mSv with current equipment. These effective doses may be compared to an average effective dose from natural background radiation of ~ 3 mSv per year, as well as with current US regulatory dose limits of 50 mSv per year for radiation workers (e.g., radiologists and medical physicists), 1 mSv per year for members of the public, and 5 mSv to the foetus of a radiation worker.
More importantly, patient effective dose from CT should be compared with other diagnostic examinations that utilise ionising radiations, including cardiac catheterisation and those involving the administration of radiopharmaceuticals. Representative effective doses for cardiac catheterisations are 5 to 10 mSv, and average patient doses in nuclear medicine examinations are ~ 15 mSv for 18F cardiac PET, ~ 20 mSv for a rest/stress 99mTc labelled Sestamibi procedure, and ~ 40 mSv for a 201Tl scan.
Some of these tests are quite liberally prescribed in daily practice; however, the radiation associated with them has largely escaped public attention.
It has been suggested that radiation risks in cardiac CT can exceed 1%, where this value was computed for a 20-year-old female patient receiving ~ 29 mSv. However, pursuant to the nature of atherosclerotic disease, the typical patient population who undergoes coronary CT angiography has a median age of ~ 60 years. Increasing a female patient’s age from 20 to 60 years would reduce the breast cancer radiation risk by over an order of magnitude. A uniform whole body dose of 20 mGy to a 60-year-old, which corresponds to an effective dose of 20 mSv, has an average radiation risk of induced cancer of ~ 0.1%. For 60-year-old women the risk is about 40% higher than that of men at that age. The average cancer risk for an effective dose of ~ 20 mSv may be compared with US population cancer incidence (42%) and mortality (22%) in 2007 as provided by the American Cancer Society.
It is important to re-emphasise that current radiation risk estimates are based on extrapolation of data derived from atomic bomb survivors and other sources, and have never been directly observed for any population exposed to CT radiation. Accordingly, it is well recognised, by all leading authorities on this topic (i.e. BEIR, UNSCEAR and ICRP), that there are very large uncertainties associated with any risks that are generated at doses of ~ 20 mSv.
Medical practice deals with individual patients where it is important to bear in mind that it is the same individual who receives the benefit as well as bearing (any) radiation risk. Under these circumstances, the key question that needs to be posed is whether our usage of ionising radiation associated with diagnostic examinations is appropriate. An appropriate answer to this question should make use of the latest principles of radiation protection practice - justification and optimisation. Justification requires an examination to be performed only when indicated, which requires that the patient benefit to exceed (any) radiation risk. For any indicated examination, optimisation requires that no more radiation should be used than is needed to obtain the diagnostic information.
In clinical practice, examinations should keep patient doses As Low As Reasonably Achievable (ALARA) and eliminate unnecessary radiation. Focusing on these two radiation protection principles maximises the benefit to our patients and minimises radiation risks. Ignoring the benefit side of the risk/benefit equation, as happens when only the magnitude of the radiation dose (and corresponding risk) is addressed and disseminated in the general public through the lay press, does a disservice to our patients.
Real harm could be inflicted on any individual patient who was deterred from having an indicated examination that provides valuable diagnostic information affecting important patient management decisions. If used responsibly and appropriately in a patient who would otherwise undergo cardiac catheterisation with the small, but very real risk of severe complications, the benefit from the non-invasive nature of CT substantially outweighs the theoretical cancer risk from ionising radiation. Accordingly, the pendulum may have swung too far in our current discussion on radiation risk and increased efforts at educating patients and referring physicians on the risk/benefit ratio of non-invasive imaging are in order. On the other hand, the individual assessment of the patient’s risk/benefit ratio and the commitment to keep radiation exposure at a minimum is incumbent on us as the stewards of radiation at medical imaging. Accordingly, all means to lower radiation dose at cardiac CT are welcome and should be utilised. There are time-honoured approaches such as ECG-dependent tube current modulation and use of lower tube voltage in younger, slimmer individuals, which should be used whenever possible.
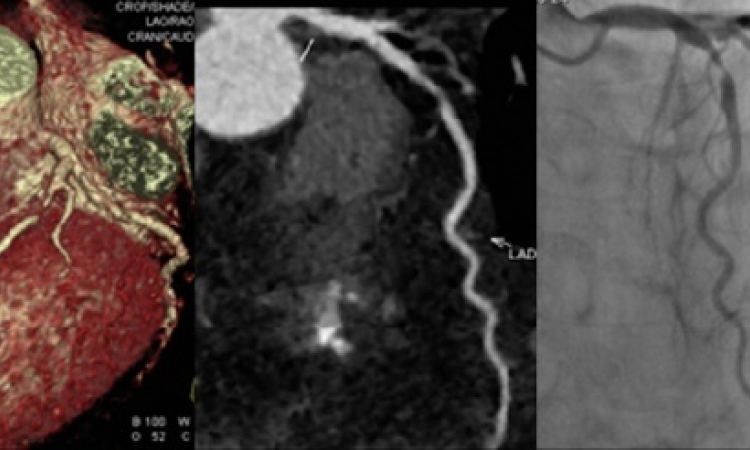
However, the most profound radiation dose savings have been reported with the recently rediscovered technique of prospectively ECG-triggered coronary CT angiography. This technique comprises sequential acquisition of transverse sections with application of radiation only during a predetermined interval during the cardiac cycle (ordinarily diastole) and had been the default method for ECG-synchronisation of scan acquisition with electron-beam CT. Compared with the constant application of radiation during slow pitch spiral acquisition inherent to retrospective ECG-gating -- the most widely used method for ECG-synchronisation with MDCT -- prospective ECG-triggering enables performing coronary CT angiography at a fraction of the effective radiation dose equivalent (i.e. 1-4 mSv).
The main limitations of prospective ECG-triggering have been the inability to evaluate cardiac function and, more importantly, to retrospectively (i.e. after an acquisition) change the co-registration of image data with more suitable phases of the cardiac cycle, which is one of the hallmarks of retrospective ECG-gating. Also, patients with arrhythmia have traditionally not been eligible for prospectively ECG-triggered examinations because arrhythmia naturally precludes reliable co-registration of image data with the desired cardiac phase.
There are various technical attempts at improving the robustness of this acquisition technique vis-à-vis faster and more irregular heart rates. These include prolonging the acquisition interval during the RR-cycle to provide more flexibility in choosing the most suitable phase of image reconstruction, or adaptive online monitoring of the ECG for the occurrence of extra-systoles in order to ensure image acquisition only during the desired cardiac phase.
As always, scanner technology is rapidly evolving and the heightened awareness regarding radiation exposure already has accelerated the development of instruments and acquisition strategies that are capable of imaging the heart at much lower radiation dose than current CT systems. The newest CT scanner generation, for instance, enables routinely imaging the heart within a single diastolic phase (i.e. ≈ 250 msec) and a radiation exposure of less than 1 mSv. The embrace of this and future low-radiation dose technologies along with careful individual consideration of the risk/benefit ratio and increased efforts at patient and physician education likely represent the best strategies for ameliorating prevailing radiation worries associated with cardiac CT.
24.05.2010