© luchschenF – stock.adobe.com
News • Achieving and maintaining high service quality
QA in histopathology laboratories from pre- to post-analytic phase
The medical field is inherently susceptible to errors, with laboratory tests being no exception.
In a new publication in the Journal of Clinical and Translational Pathology, Prof. Mohammad Mubarak from the Sindh Institute of Urology and Transplantation, Karachi (SIUT) in Pakistan details on the various phases of quality control (QC) and quality assurance (QA).

Image source: Mubarak M, Journal of Clinical and Translational Pathology 2024 (CC BY-NC 4.0)
In histopathology laboratories, where tests are considered the gold standard for diagnosing various diseases, errors can significantly impact patient outcomes. QC and QA programs are essential in minimizing these errors and ensuring the generation of accurate and reliable reports. The complex, multistep nature of histopathology work, combined with the subjective nature of many diagnostic interpretations, makes implementing QC methods challenging yet crucial. Implementing effective QA and QC measures ensures that histopathology laboratories adhere to the highest standards of diagnostic accuracy and reliability, thereby safeguarding patient health and enhancing clinical outcomes.
The primary objectives of quality schemes in histopathology laboratories include producing accurate and complete test reports, delivering these reports promptly, maintaining high ethical and professional standards, and providing continuous education and training to laboratory staff. These objectives are vital for achieving and maintaining high-quality services in histopathology. By adhering to these quality objectives, histopathology laboratories can ensure that diagnostic processes are not only accurate but also efficient, fostering trust and reliability in laboratory results.
The testing cycle in histopathology laboratories is divided into three main phases: pre-analytical, analytical, and post-analytical. Each phase involves specific processes and quality control measures to ensure accurate and timely results. The careful management of each phase is crucial to minimizing errors and ensuring that the diagnostic process is seamless from start to finish.
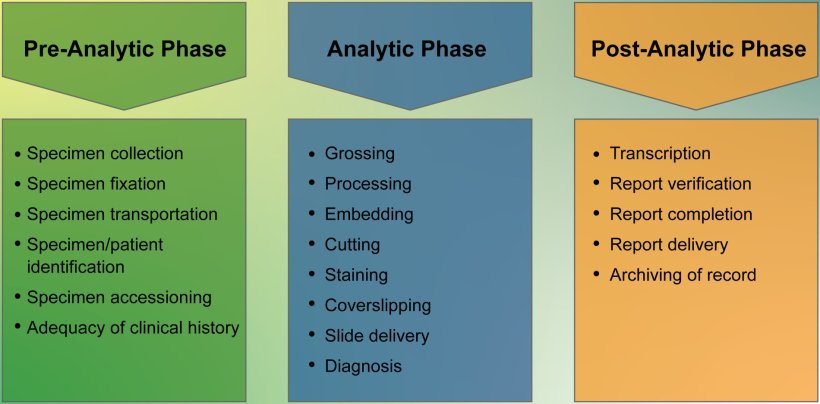
Image source: Mubarak M, Journal of Clinical and Translational Pathology 2024 (CC BY-NC 4.0)
Pre-analytical phase
The pre-analytical phase is critical as most errors occur during this stage. Accurate patient and sample identification is paramount. Errors in this phase can affect all subsequent steps. The involvement of multiple personnel, including those outside the laboratory, necessitates a comprehensive organizational effort to improve this phase. Quality assurance monitors for this phase include labeling errors, adequacy of clinical history, and lost specimens. Effective communication and coordination among all parties involved in this phase are essential to mitigate the risk of errors and ensure that samples are handled with utmost care and precision.
Analytical phase
The analytical phase involves the technical and interpretative steps necessary for diagnosis. There is some debate about the exact scope of this phase, but it generally includes gross examination, processing, embedding, cutting, staining, and ultimately, diagnosis. Peer review is a critical quality measure in this phase due to the subjective nature of histopathology reporting. Both prospective and retrospective methods are used to ensure accuracy and reduce errors. The implementation of robust peer review mechanisms ensures that diagnostic interpretations are subjected to rigorous scrutiny, thereby enhancing the accuracy and reliability of laboratory results.
Post-analytical phase
The post-analytical phase ensures the completeness and accuracy of reporting, including transcription and report corrections, verification, and correlation with ancillary studies such as immunohistochemistry (IHC) and electron microscopy. This phase also covers the timely delivery of reports to clinicians and patients. Ensuring that reports are accurately transcribed, verified, and delivered on time is crucial to maintaining the integrity of the diagnostic process and facilitating effective clinical decision-making.
Turnaround Time (TAT) TAT and clinician/patient satisfaction are important parameters for assessing laboratory performance. Timely reporting and high satisfaction levels indicate effective quality management in histopathology laboratories. Monitoring and optimizing TAT not only improves operational efficiency but also enhances patient care by providing timely diagnostic information to clinicians.
External Quality Assessment (EQA) schemes, clinical audits, continuing medical education, and laboratory accreditations are crucial for maintaining and improving diagnostic standards. These activities provide educational value and feedback, helping laboratories recognize and rectify performance issues. Participation in EQA schemes is often optional but highly beneficial for continuous improvement. Engaging in these external assessments fosters a culture of continuous learning and quality enhancement, ensuring that laboratories stay abreast of best practices and emerging trends in the field.
Achieving and maintaining high-quality services in histopathology laboratories require coordinated efforts from all stakeholders. There is a need to increase awareness about the importance of QA&I schemes among pathologists and other healthcare members to ensure optimal patient care. By fostering a collaborative and quality-focused environment, histopathology laboratories can significantly enhance diagnostic accuracy, reduce errors, and ultimately improve patient outcomes.
Source: Xia & He Publishing Inc.
09.09.2024