Precision medicine will transform reporting, reimbursement
Nothing is more personal than a scan of the insides of your body. Yet radiology images today look a little old-fashioned and out-of-step in the fast-emerging movement to personalised medicine.


The leading edge of patient-focused diagnosis today is what Hans-Ulrich Kauczor, M.D. called an explosion of fresh insights from genomics, metabolomics, proteonomics, the so-called -omic data, that he says is radically changing the face of modern medicine by creating highly personal patient profiles that facilitate individualised diagnosis and treatment.
Yet what we learn from omni-omics is not something that can be relied upon to make clinical decisions, he said.
"These personal evaluations will give you a risk profile. You may learn, for example, you have a 10-fold higher risk than anyone else to develop a certain condition. In fact your statistical risk of actually developing that condition remains quite low," said Kauczor. By comparison, medical imaging at a minimum provides a specific diagnostic assessment of your condition with upwards of 80% sensitivity and specificity.
The role that radiology can play, perhaps as radio-omics, will be the focus for a special New Horizons session this year at the European Congress of Radiology, called Imaging in Precision Medicine.
European Hospital spoke with Prof. Kauczor about the coming transformation of traditional radiology to join the universe of -omic diagnostics and treatment.
EH: What are the challenges in personalising radiology?
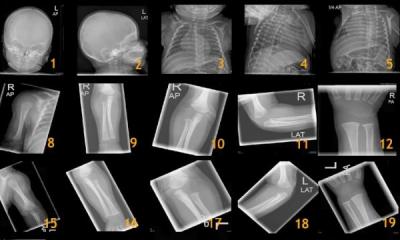
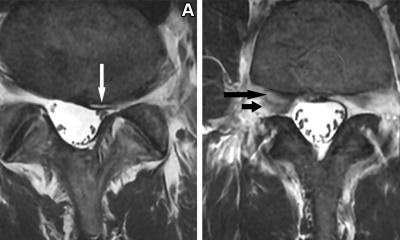
Kauczor: We need standardization with common protocols, common read outs. At the congress there is a lot of science. For example there will be many presentations showing how great perfusion MRI is today. Yet if you go to 10 different tertiary hospitals, there will be 10 different protocols with scanners of different generations from different vendors. We have to find a basis of simple but robust measures to come up with reasonable, consistent results. We need a robust, shared base of data.
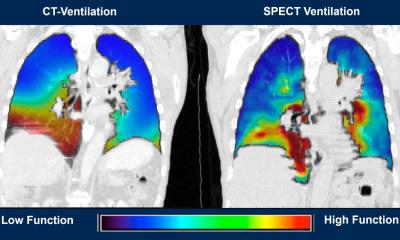
Precision radiology needs to drive the change to personalized medicine from today's radiology reporting that has a lot of prose and lots of variations in the prose with different terms and meaning found between the lines. This is not helpful for personalized medicine. We need precise measurements to form the backbone of a structured report, giving size, density, intensity, rates of perfusion or diffusion.
Can a radiologists provide this precision, or do we look to automate this data collection?
It has to be a machine. Radiologists would take too long, and perhaps be subjective in choosing regions of interest and so forth. Here we need pre-processing of images, with quantitative read outs, measurements, and perhaps color-coding of objects that we can turn on and off. The radiologists can then review the original images, the pre-processed images, the post processed images, the quantitative read outs, and makes a diagnosis.
In other words, to personalise medicine, we will de-personalised radiology?
In medicine, especially in personalised medicine, we can not leave the machines alone talking to each other. Someone needs to generate evidence, guidelines and standards. Some of these can be implemented in a machine that runs on these rules. Someone needs to decide how to direct the patient, to which protocols. And then every image is going to have highly personal locations, density and distributions that will never be perfect for machine reading. We need machine support in radiology. But it is the radiologist who takes the decisions in the end. As with other medical disciplines, we need to be close to the patient. And we must remain the masters of the machines in the process.
Who is going to pay for all this change to processes and machines?
In the end the standard of radiological exam should be redefined. Currently there is the so-called unity of image and report. We are reimbursed for the image and a report in prose. There are very low standards regarding the reporting requirements. We need to take the next step and say there is certain content and measurements in a radiology report, and for this reason it should be reimbursed at this level. Money drives the entire system, and reimbursement needs to reflect any requirement for a change in quality for reporting standards. In this way, if a report does not meet the standards, it would not be reimbursement. This is the only way to introduce change.
06.03.2014