Peering into the abyss
In May, the World Health Organisation (WHO) warned that bacterial infections might lead to an increasing number of deaths because new resistance mechanisms threaten our ability to treat common infectious diseases.

One factor accelerating the evolution of resistance is the incorrect or excessive use of antibiotics.
This June, the emergence of resistance, or rather its avoidance, was the focus of the 12th Congress on Infectious Diseases and Tropical Medicine (KIT). With around 1,000 participants, KIT is the largest event of its kind in the German-speaking countries, traditionally following an interdisciplinary approach, integrating areas such as microbiology, hygiene and internal medicine.
‘Resistant bacteria are an increasingly important issue not only in hospitals but also in out-patient facilities. Although we do make progress in terms of avoidance, the non-development of new anti-infection drugs, particularly antibiotics, is utterly incomprehensible in view of the rapid emergence of new resistances,’ says KIT President Professor Jan van Lunzen, from the University of Hamburg.
In light of this, the appropriate use of antibiotics as well as avoidance of superfluous antibiotics prescriptions are crucial – and can only be guaranteed by specifically trained infectiologists who bring comprehensive clinical experience to the therapy team.
However, infectiology as a clinical specialty is rare and known to very few physicians. It combines elements from microbiology and hygiene, ideally, is integrated into patient care. ‘Today, patients are presenting with highly complex diseases that cannot be treated as easily as some people claim. Even the assessment as to whether we are dealing with an infectious disease, or not, as well as differentiation from other diseases, can be extremely difficult. We are frequently called in when our colleagues from other disciplines are at a loss,’ explains Professor Dr Gerd Fätkenheuer, Chairman of the German Society for Infectiology and consultant at the infectiology out-patient department at Cologne University Hospital.
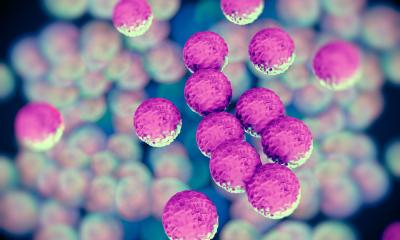
The benefits of infectiological advice are well documented: Five years ago a study conducted at the University of Freiburg had already indicated that the mortality rate of staphylococcus aureus infections can be reduced from 43 to 28 percent when infectiologists are part of the clinical team.
Thus Professor Fätkenheuer and colleagues demand more infectiologists in the country’s hospitals. ‘In Germany we have three to five infectiologists per million residents. Europe-wide we rank in the lower third. By comparison: Sweden counts 20 to 25 infectiologists per one million residents.
‘For any facility with 500 beds and upward, a fulltime infectiologist should be mandatory. In facilities of this size this is economically feasible and enhances the quality of care,’ Fätkenheuer emphasises.
Professor Winfried V Kern, senior physician at the Centre of Infectiology and Travel Medicine at the Albert Ludwig University Freiburg, and initiator of the new comprehensive guideline (German classification S3) to ensure rational hospital antibiotic prescription, calls for an infectiology act similar to the amended German Protection against Infection Act of 2011 for hygiene. This act, Kern says, created an excellent and countrywide staff and structural framework for modern infection prevention. ‘It would have been very nice if we had been able to include the therapy aspect in the act, but it was too early for us. In the end the statutory refinancing options provided for prevention have to be made available for therapy as well. This is the only way to ensure that we can reach the minimum target of 1,000 hospital-based infectiologists up from the current 300,’ Kern points out.
To attract more physicians to this specialty, a four-pronged approach is needed: more university chairs, more hospital positions, better training and more and better career options.
An important step in the right direction is the new Austrian-German guideline, classified as S3, which is based on a systematic literature search and assessment of evidence.
According to the guideline, the key component to improve the quality of hospital antibiotic prescribing is the so-called Antibiotic Stewardship Team (ABS team), an interdisciplinary group headed by an infectiologist. ‘Most clinicians cannot fully assess infections because the diseases are becoming ever more complex. If specialists such as infectiologists are not integrated into the therapy, the therapy has gaps.’
The ABS team is strategically oriented and looks beyond the individual case. Data on antibiotics consumption and data from infection registries, which record infections caused by resistant pathogens, can be analysed to assess the prescription quality. Based on the results, hospital-specific antibiotic prescription guidelines can be initiated.
In such a scenario, hospital pharmacists, specialist physicians in microbiology as well as hospital hygiene experts cooperate closely with the ‘antibiotics officer’ of each department.
‘Such an investment in specialists will more than pay off,’ Kern believes. ‘It will most likely reduce costs for pharmaceuticals in an amount that’s far higher than the personnel costs, not to mention the immense benefits in terms of patient safety and the long-term benefit of reining in the emergence of resistances. This,’ he emphasises, ‘is the only way to ensure successful therapies in the future. If we don’t get a grip on the resistance issue, we are jeopardising medical progress.’
04.09.2014