Patient's brain controls mechanical ventilation
Among ventilation advances demonstrated at this year's European Society of Intensive Care Medicine Congress, held in Barcelona, the combination of the SERVO-i ventilator with Neurally Adjusted Ventilatory Assist (NAVA) provoked considerable interest because the system allows ventilation to be controlled by the patient's own respiratory centre in the brain. During a discussion with Daniela Zimmermann, Östen Olsson, the Marketing Director for Ventilation at MAQUET Critical Care, described the development and effects of this ground-breaking technology.

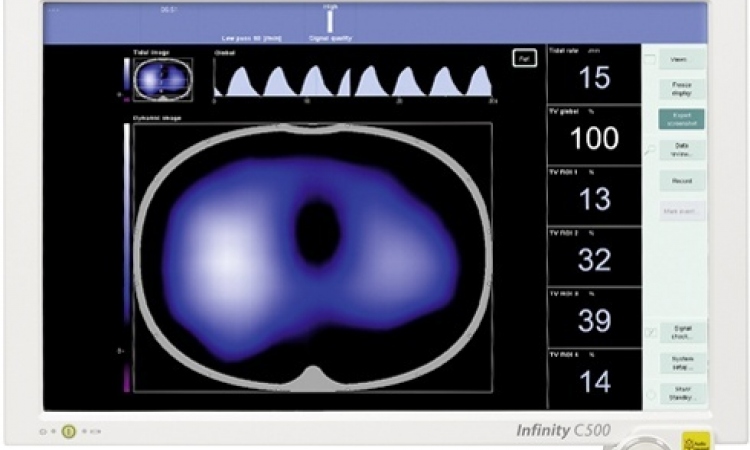
ÖO: The respiratory centre in our brains manages our respiration, by sending signals via the phrenic nerve to the diaphragm, where the signals are transformed into breathing activities. Conventional mechanical ventilation systems sense a patient’s breathing by either a drop in airway pressure or reversal in flow – the last and slowest reaction in the chain of respiratory events. With NAVA a catheter catches signals sent by the brain to the diaphragm and provides the ventilator with an electrical activity of the diaphragm (Edi) signal. This means we are able to detect breathing demands before the breathing action take place and therefore can affect the ventilation in synchrony. So ventilation is based on the patient’s neural respiratory output and it also assists the patient’s breathing in a proportional way. For clinical practice, this really means a paradigm shift.
Because the body itself gives the signal, the ventilator provides the patient with exactly the amount of air needed. There is no over or under assistance and therefore the lungs are protected. Moreover, we have improved synchrony between patient and ventilator. The Edi signal, a new parameter in mechanical ventilation, provides important information for diagnostic purposes by monitoring electrical activities. For example, it can be used as a tool for clinicians to interpret the background of the chaotic breathing pattern so often seen in the infants. Direct access to the respiratory centre output gives prompt information on the effect of any intervention relating to ventilation of the lung.
Due to a disease, could the patient’s control centre send the wrong signals - perhaps that more oxygen is needed, yet the opposite would be better?
ÖO: The worse the disease is, the higher the signals output, and the ventilator automatically assists more. Most diseases lead to a reduction in a patient’s breathing efforts. The signal only influences the ventilatorion, thus keeping the system working to compensate the difference in ventilator support needed. That is the sophisticated point!
The idea of neurally controlled ventilation first arose in the mid-80s. Twenty years later you are presenting the first result in this technology. What happened in the intervening years?
ÖO: The basic research began in the mid-80s at the University of Gothenburg. In the beginning it was not focused on mechanical ventilation of patients; it was only for research purposes on muscle EMG (electromyographic) signals. This idea to involve mechanical ventilation came later on. At that time, the pacemaker industry was also already working on the idea of trying to assist the diaphragm with an electrical signal. But they soon gave in, because they recognised there were really complicated processes involved.
We started our investment at the beginning of the 2000, when we saw progress in technologies. However, as you see, it took a while until the technique was reliable.
If we look at the history of ventilation, NAVA can be a paradigm shift in mechanical ventilation technology. In the 50s, mechanical ventilators were heavy machines, really pumping air into the patients. During the 70s and 80s the spontaneous breathing method began to improve, which was a great progress because patients could interact far better. The focus in the 90s was on protective ventilation, meaning not to harm a patient and cause trauma. Now the body can speak for itself and we may have a self-regulating technology.
What might we see in the future?
ÖO: This new technology gives us a lot of impetus for research because now we can generate information that we never had before.
16.11.2006