Article • Brain tumour resection
Navigated ultrasound - The best intraoperative imaging technique
New navigation imaging and neurophysiological stimulation techniques enable an approach to brain tumours long considered unresectable before and during surgery, but not one does it quite as well as ultrasound, according to a leading Spanish neurosurgeon.
Report: Mélisande Rouger

Resecting an entire tumour and determining brain shift remain challenging for surgeons in brain cancer surgery. However, they are likelier to overcome these difficulties if they use intraoperative ultrasound, according to Dr Cristian de Quintana, neuro oncologist at Santa Creu i Sant Pau Hospital in Barcelona. ‘Neuro navigated ultrasound provides the surgeon with confidence in the assessment of resection accuracy and in the determination of brain shift,’ he said. Last August, during the World Congress of Neurosurgery in Istanbul, de Quintana presented the results of a prospective two-year study on ultrasound use in intra-axial tumours.
For surgeons, brain shift is a major problem. Even if they use pre surgical imaging to help plan surgery, the brain will change during the intervention; it will lose liquid and volume, shift shape and move, and ultimately make it harder for surgeons to perform.
Unlike intraoperative magnetic resonance imaging (MRI), which requires 20-30 minutes time to adjust to pre-surgical images, it takes a little over two minutes (2 minutes 19 seconds) for intraoperative ultrasound to overlap with previous images. Because it is so fast, ultrasound can be repeated as many times as necessary, enabling the surgeon to detect brain shift and evaluate how much tumour is left, almost instantly. ‘Ultrasound has changed the way we operate on patients. When I’m done resecting, I check if the tumour has been fully removed, or if there is any residual. In 14% of the cases, ultrasound helps to resect further, which significantly improves our results. Extensive resection tremendously increases patient survival and prognosis,’ de Quintana pointed out.
Ultrasound is not a complicated technique, but you need good equipment and good probes
Cristian de Quintana
Intraoperative imaging enables to safely excise tumours long thought to be unresectable. At Santa Creu i Sant Pau Hospital, ultrasound has helped de Quintana to successfully carry out surgery in 10-20 patients of the 40-50 patients he operates on annually. Another benefit of ultrasound compared to other intraoperative techniques is that it is cheap and easily moveable across the hospital, without losing too much in image quality. After studying hundreds of cases over two years, de Quintana observed that ultrasound had achieved 78% of correlation with pre-surgery MRI. ‘That’s a totally acceptable performance for intraoperative imaging,’ he confirmed. Ultrasound is particularly helpful in visualising metastases, which are less infiltrative than glioma and usually easier to resect.
Last but not least, the learning curve is much faster than with MRI. ‘All you need is a bit of experience. Ultrasound is not a complicated technique, but you need good equipment and good probes.’ All these benefits have convinced the researcher that ultrasound is the best imaging tool in his arsenal. ‘Based on image quality, time, ease of use and cost, ultrasound is the most efficient intraoperative imaging technique at our disposal.’

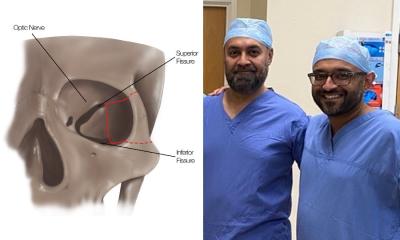
Nevertheless de Quintana stressed the role of functional MR and tractography in the pre surgical setting. ‘We are increasingly using these techniques to help prepare for surgery,’ he said. ‘They remain crucial to be able to localise tumour and determine our approach, in order to resect as much tumour as possible without damaging neurological function.’ Tractography, in particular, is instrumental in visualising subcortical neural tracts and understanding how the tumour relates to surrounding structures. The technique relies on 3-D modelling based on data collected by diffusion-weighted images, and uses colour to image functions such as language, vision and motion. This information is then sent to the neuro navigator to facilitate surgery.
De Quintana also highlighted the role of neurophysiological stimulation during surgery to help distinguish functional areas of the brain and evaluate patient response. Brain mapping in tumours located in or close to key areas generating motion, vision and speech or linked to memory enables assessment of response while the patient is awake or asleep. A surgeon, neurophysiologist and neuropsychologist usually perform this stage of treatment together. Once the patient is asleep, the medical team will gently wake him or her up to perform brain mapping and ask him/her to carry out tasks. Doctors then perform tumoural resection, and close up the patient when he/she is asleep or sedated.
Profile:
Cristian de Quintana is responsible of neuro-oncology in the department of surgery at Santa Creu i Sant Pau Hospital in Barcelona. He is a specialist in highly complex brain tumour resection and an expert in technological advances in this field. His publications, courses and conference presentations number more than a hundred.
14.11.2017