MRI and plaque imaging
Cardiovascular disease is the leading cause of death in industrial nations. More than 50 percent of those deaths are associated with pathologies of the coronary arteries, despite the fact that luminal obstructions that lead to myocardial infarction or ischemia do not occur out of the blue. The initial symptoms are preceded by a whole slew of arteriosclerosis stages and the early detection of these could prompt treatment to slow, stabilise or even reduce the disease.

Photograph: Rainer Sohlbank
However, such early detection would involve diagnostic examinations of healthy and thus far asymptomatic people – which therefore precludes invasive procedures and those that entail ionised radiation. MRI might offer a feasible alternative, according to Professor Matthias Stuber, Director of the Centre for Biomedical Imaging (Centre d´Imagerie BioMédical – CIBM*), in Lausanne, Switzerland, in his presentation MRI in Plaque Imaging for this year’s ESC. Interviewed by Meike Lerner, he addressed the question of whether MRI in plaque imaging is a clinically relevant tool or just a toy for the research community
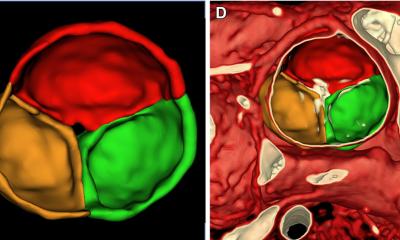
‘Today, arteriosclerosis assessment via MRI is mainly limited to research. However, there are initial studies evaluating the benefits of the method to quantify plaque and its progression in animal models and human patients. Moreover, we try to analyse the composition of the plaque, which is an important issue with regard to establishing risk profiles, since many of the stenoses that rupture are in regions that don’t show significant disease in heart catheter images’ Professor Stuber explained.
Today, such MRI applications are technically rather demanding in terms of the technology, particularly in terms of system operation and thus the training for radiographers. There is also another obstacle to surmount, he said. While manufacturers can produce contrast media that may show different plaque components, due to regulatory issues their research and development efforts have cooled down considerably. Nevertheless, according to this expert, MRI in plaque imaging may well make it into clinical practice: ‘Technology will make use of MRI so that the early detection of arteriosclerosis is possible, although it remains to be seen who will pay for such a procedure and for which patient groups the procedure should be indicated.’
No matter how these decisions are to be made in the future, today the method has already demonstrated its value. ‘Non-invasive and radiation-free diagnostics provided us with many insights into arteriosclerosis, particularly in its early stages. Today, we can also examine younger individuals and not have to wait until the patient presents with symptoms in the cath lab.’
As to whether MRI for plaque imaging is a tool or a toy, Professor Stuber said: ‘It depends… There is a clear difference between applications that are already being used, and thus will become clinical tools shortly, and research projects experimenting with contrast media that are perfectly suited for visualisation purposes but which are clearly toxic and thus will probably remain as mere research toys’.
* The CIBM aims to advance our understanding of biomedical processes in health and disease, focusing on mechanisms of normal functioning, pathogenic mechanisms, characterisation of disease onset prior to structural damage, metabolic and functional consequences of gene expression, and non-invasive insights into disease processes under treatment. The research will use model systems ranging from transgenic animals to human patients (‘from mouse to man’) and foster multi-disciplinary collaboration between basic science, biomedical science and clinical applications.
26.08.2011